Clinical Aspects of Adrenal Disorders Flashcards
(66 cards)
What does each layer of the adrenal glands secrete?

What are the classification of adrenal disorders?

Explain the common approach to treating adrenal disorders?
- Clinical suspicion
- Test for assessing functional status
- Is it functioning
- Is it primary or secondary
- What is the aetiology
- If tumour
- Can it be removed
- Would chemotherapy and radiotherapy help
Endocrine deficiency needs correction
What does HPA stand for?
Hypothalamus-pituitary-adrenal axis

What impact does hypofunction have on the HPA?

What can hypofunction of the adrenal glands be caused by?
- Primary adrenal insufficiency
- Addison’s disease
- Immune destruction
- Invasion
- Infiltration
- Infection
- Infarction
- Iatrogenic
- Adrenal enzyme defect
- Congenital adrenal hyperplasia (most commonly 21-hydroxylase deficiency)
- Addison’s disease
What are some causes of Addison’s disease?
Immune destruction
Invasion
Infiltration
Infection
Infarction
Iatrogenic
What enzyme most commonly causes adrenal enzyme defect?
21-hydrolase deficiency
What does adrenal enzyme defect cause?
Congenital adrenal hyperplasia
What autoantibodies are looked for in Addison’s disease?
Positive adrenal autoantibodies to 21-hydroxylase
How is the adrenal cortex involved in Addison’s disease?
Lymphatic infiltrate of adrenal cortex
Addison’s disease is often associated with other autoimmune disease, what are some examples?
Thyroid disease
Type 1 diabetes mellitus
Premature ovarian failure
What are some common symptoms of primary adrenal failure?

What are some clues to a diagnosis of adrenal failure?
- Disproportion between severity of illness and circulatory collapse/hypotension/dehydration
- Unexplained hypoglycaemia
- Other endocrine features (hypothyroidism, body hair loss, amenorrhoea)
- Previous depression or weight loss
What is the most common cause of adrenal failure?
Autoimmune Addison’s disease
What is done to diagnose adrenal insuffiency?
Routine bloods (U and Es, glucose, FBC)
Random cortisol
Synacthen test (and basal ACTH)
What routine bloods are done when investigating adrenal insuffiency?
U and Es
Glucose
FBC
For a random cortisol test, what level is not an Addison’s diagnosis?
>550nmol/L
For a random cortisol test, what level is potentially an Addison’s diagnosis?
<500nmol/L
Is Addison’s disease a cause of hyper or hyposecretion of the adrenal glands?
Hyposecretion
What is the synacthen test?
Special chemical test to see how well adrenal glands make cortisol
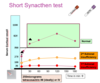
Explain the process of diagnosing adrenocortical insuficiency?

What medicines can be used as glucocorticoid replacement?
- Hydrocortisone 20-30mg
- Prednisolone 7.5mg
- Dexamethasone 0.75mg
What can be used as mineral corticoid replacement?
Synthetic steroid called fludrocortisone



















