CNS1 General anaesthesia, local anaesthetic and resucitation Flashcards
(16 cards)
Which are the three importand anaestetic drugs?
ether
nirous oxide (Stickstoffoxid)
chloroform
What are the preoperative assessment of the patient before applying anaesthetics?
- measurement of blood pressure and heart rate
- check the veins for ease of canulation
- examination of the lungs, including chest X-rays if indicated
- ECG if indicated
- examination of any cartoid bruit
- identification of heart murmurs
- test for heamoglobinopathy as appropiate
- check for impaired mobility of the temporomandibular joints and for rheumatoid arthritis associated mobility problems of the neck
- blood tests, including liver function tests
What is premedication (Praemedikation) and why is it necessary?
Premedication is the administration of drugs to patients an hour or two before anaestesia and surgery. The objectives of premedication are:
- relieve anxiety
- reduce the production of saliva
- reduce the volume, and increase the pH, of the gastric content.
Name 6 anxiolytic drugs (DE: Anxiolytikum, angstmildernd)
- Temazepam (orally)
- Midazolam (orally)
- Diazepam
- Lorazepam
- Alimemazine (orally)
- opioids such as morphone (just given to patients in pain before surgery)
Name 3 drugs which reduce salivary secretion
- atropine (das Atropin, intramuscular injection, also orally given but the dose must be twice as much)
- glycopyrronium (Glycopyrroniumbromid, intravenously)
- hysocine (no longer used because it may cause confusiion and restlessness)
Name 3 drugs which reduce the volume and increse the pH of gastric contents
- metoclopramide (DE: Metoclopramid) (orally or intravenously) hastens gastric emptying
- sodium citrate (Natriumcitrat) (orally) raises the pH of gastric content by neutralizing acid in the stomach
- ranitidine (DE: Ranitidin) (orally or intravenously) raises the pH of gastric secretions
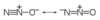
Explain the properties of nitrous oxid (DE: Distickstoffmonoxid)
weak aneastesia
you have to inhale it
faintly smelling and stored as a liquid
needs to be combined with other analgesic because it is very weak
Anastetic containing nitrous oxid
Entonox
- 50:50 mixture of nitrous oxide and O2
- used for pain relief in labor, by ambulance crews
Which is the most commonly used inhalational anaestetics?
Isoflurane (DE: Isofluran) which belongs to the halogenated hydrocarbons. It has little effext on cardiac output and is associated with a repid recovery from anaestesia.

What are the positive sided of opioid analgesics?
- little effect on blood pressure and cardiac output
- short acting
- most commonly used are fentanyl (30 min), alfentanil (10 min), remifentanil (a few minutes)
Why do most anaesthetics react as muscle relaxants?
to facilitate intubation of the trachea with an endotrachela tube at the beginning of anaesthesia
to relax muscles sufficiently to make surgery possible (especially in abdominal surgery)
to permit artificial ventilation
What is curare (DE: Curare)?
It is a tropical plant in South America and its alkaloid is used as a muscle relaxants.

How does a muscle relaxant work on a neuromuscular junction?
Muscle relaxants act at the neuromuscular junction by blocking the transmission of nerve impulses from the nerve to the muscle.
Name the 2 groups of muscle relaxants which are competitive /non-depolarizing blockers
Aminosteroid group: pancuronium, rocuronium, vecuronium
Benzylisoquinolinium group: atracurium, cisatracurium, gallamine, mivacurium
What is suxamethonium?
It is a depolarizing muscle relaxant. It occupies the receptor sites for acetylcholine and initially stimulates the muscle into contracting, visible twitching or fasciculation that occurs almost immediately after it is injected.
Special points:
- quick onset of action, ca. 60 seconds, it is used in patients who may have full stomachs in whom rapid tracheal intubation is indicated
- short duration of action, ca. 5-10min
- rapidly broken down
- side effect is muscle pain
How can the effect of muscle relaxants be reversed?
By using anticholinesterase. Anicholinesterase act at the neuromuscular junction, where they temporarily inhibit the enzyme cholinesterase, which normally breaks down
acetylcholine, and allow the concentration of acetylcholine to rise and so help the return of normal neuromuscular transimission mucle strength. But anticholinesterase is associated with the following side effect:
- increseof salivation and tracheobronchial secretions
- bradycardia
- increase if peristaltic activity in the gut→diarrhoea
Those side effects can be prevented by administering neostigmine, edrophonium.
Why are anticholinergic drugs used?
They are used during anaesthesia and have the follwing effect:
- to increase pulse rate
- to reduce tracheobronchial and salivary secretion
- to prevent the increase of peristaltic activity
How they work: block the affects of acetylcholine, particularly at postganglionic parasympathetic nerve endings.
Drugs: Atropine, Glycopyrronium


