Colitis/Colon Tumors Flashcards
(38 cards)

Normal colon

Diverticulum; outpouchings of colonic mucosa and submucosa; common in US population (low fiber diet), can be plugged with stool, get secondarily inflammed (diverticulitis)
Active colitis; infiltration of neutrophils into surface/crypt epithelium; usually presents with diarrhea; see cryptitis (neutrophils within epithelium of crypt), expanded LP with inflammation, crypts are further apart than normal though architecture still intact.
“active colitis” is a non-specific finding; can be due to infectious colitis, IBD, or NSAID hyperinflammation

Active colitis; see intraepithelial and intraluminal neutrophils due to crypt rupture

Infectious colitis, see cryptosporidium (blue arrows), pt presents with active colitis, take a travel hx

C. diff pseudomembranous colitis; grossly colon appears very erythematous with yellow/green pseudomembranes (made of fibrin, mucin, and inflammatory cells); can lead to sepsis/death

Pseudomembranous colitis; see pseudomemb. replace full thickness of mucosa and are comprised of a “volcano-like” extrusion of mucin, fibrin, and neutrophils.

C diff pseudomembranous colitis vs. ischemia; fibrino-purulent destruction of epithelium with neutrophils; look very similar cannot differentiate under microscope so clinical hx very important

microscopic collagenous colitis; often seen in middle-age women with chronic watery diarrhea, colonscopy is normal, by on bx see lymphocytes, plasma cells, and eosinophils in LP, damage to the surface epithelium with thickening of BM;
on trichrome stain see blue bands of collagen under surface eptihelium.

Microscopic lymphocytic colitis; chronic watery diarrhea seen more often in men, similar to collagenous colitis, prominent lymphocytic infiltrate or crypts, damage to surface epithelium, no collagen deposition; often seen related to drug rxns
Eosinophilic colitis; rare, seen in neonates and young adults, 75% with hx of allergy/atopy, often seen in pt with eosinophilic gastritis/esophagitis; ddx includes parasitic infection, drug rxn, IBD

Ischemic colitis; most cases related to atherosclerosis, pt present with rectal bleeding, abd pain or full-blown peritonitis; on microscopy see slight atrophy of mucosal crypts or even full-thickness bowel necrosis; surg intervention usually necessary
Big photo, on L see remnant crypts, on R see no surface epithelium

Chronic colitis; see crypt distortion/drop-out, plasma cell/lymphocyte infiltrates that broaden separation between MM and crypts, paneth cell and pyloric metaplasia

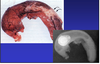
Crohn’s Dz; may affect all parts of the GI tract, most frequently the terminal ileum, often spares rectum–“Skip lesions”; see transmural (full-thickness) inflammation and fibrosis; can lead to deep fissures, fistulas, and non-casseating granulomas
complications include strictures, fistulas, and local recurrence

Crohn’s Dz; can affect all parts of the GI tract, most commonly terminal ileum, sparing rectum; see mucosal changes of chronic colitis, transmural inflammation and fibrosis, deeps fissures/fistulas, and non-casseating granulomas

Crohn’s Dz, mesenteric fat overgrowth

Crohn’s Dz; see mucosal changes of chronic colitis, transmural inflammation and fibrosis; smaller photos on bottom show non-casseating granuloma

Ulcerative Colitis; rectum always involved, see continuous inflammation confined to mucosa and submucosa, muscular wall nml, no deep fissures/fistulas, “pseudopolyps” common, rare granulomas; complications include toxic megacolon and colitis cystica profunda

Ulcerative colitis, see pseudopolyp with fibrinopurulent debris
Ulcerative colitis; low grade on L, high grade on R

MALT lymphoma—mucosal associated lymphoid tissue, B cell origins, associated with H.pylori infection

MALT lyphoma
Acute appendicitis; lifetime risk 7%, M>F, increased intraluminal pressure and decreased venous outflow, 50-80% due to overt obstruction; leads to ischemic injury, stasis, bacterial proliferation and inflammation.

Acute appendicits, see neutrophil infiltrates