Day 12 OBGYN Flashcards
(117 cards)
A 28 year old female attends her GP with her husband, who is 29.
They have been trying to become pregnant for six months.
They are both fit and healthy, are not using any contraception, and are having intercourse three to four times per week.
She is concerned she is infertile and is wondering what investigations are available to her.
What is the most appropriate initial management for this couple?
No specific medical investigations are warranted at this time
As a healthy young couple, they have a high (80%) chance of conception within one year of regular unprotected intercourse.
It is sensible to provide this couple with lifestyle advice related to conception e.g. alcohol and caffeine intake, folic acid supplementation, drug use, smoking and body weight.
A woman of reproductive age that has not conceived after one year of regular unprotected intercourse should be offered further clinical assessment and investigation, along with her partner.
A 23 year old para 1 (previous vaginal delivery) woman is brought into maternity by ambulance at 28+3 weeks with heavy vaginal bleeding and intense abdominal pain.
She reports a sudden onset of abdominal pain this morning ‘like a contraction but continuous’, unrelieved by Paracetamol.
40 minutes later she noted heavy vaginal bleeding, soaking through three sanitary pads in the last hour.
Her observations are: pulse 110, blood pressure 132/96, respiratory rate 24, SpO2 99%, temperature 37.4
She is otherwise well and has had an uncomplicated pregnancy so far.
On examination her abdomen is hard and tender and you are unable to feel foetal movements.
Dark red vaginal bleeding is ongoing.
What is the most likely diagnosis?
Placental abruption occurs when the placental prematurely separates from the wall of the uterus. This can cause profuse bleeding as the uterine vessels are sheared.
Immediate investigations in this case would involve evaluation of the foetus via either dopplar or CTG and ultrasound scan to view the uterus and look for evidence of placental abruption. Ongoing management would depend on the status of the patient, viability of the foetus and the degree of placental abruption suspected. In this case, bleeding continues to be heavy, and therefore urgent caesarean section would be considered.
A 30 year old primiparous woman who is now 41 weeks pregnant is seen in the antenatal clinic by the midwife.
She has had an uncomplicated pregnancy so far and all bloods and scans have been normal.
There has been no rupture of membranes.
On examination the symphysis-fundal height is 40cm, the fetus is cephalic presentation and the head is 2/5 palpable.
The mother explains that she is “fed up” and hopes that she goes into labour soon.
Which is the next most appropriate step in her management?
She should be offered a cervical membrane sweep to try and stimulate spontaneous labour
A cervical membrane sweep increases the likelihood of spontaneous labour initiating as it causes release of prostaglandins.
A 31 year old woman attends her booking visit at 10 weeks gestation.
This is her first pregnancy and other than some morning sickness she has had no vaginal bleeding or other problems so far.
The results of her booking bloods come back which show no abnormalities, but her Rhesus status is found to be negative.
She is worried that she will need injections.
Which of the following is the most appropriate management?
Give anti-D immunoglobulin at 28 weeks.
National guidelines advise one 1500IU dose of anti-D immunoglobulin at 28 weeks gestation, with further doses if sensitising events occur (such as heavy vaginal bleeding, amniocentesis, delivery and external cephalic version).
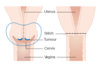
Facts about placenta praevia
(4)
A digital vaginal examination should not be performed with known placenta praevia as it can cause massive haemorrhage.
Bleeding from placenta praevia is usually painless and rarely fatal. It presents after 20 weeks of gestation.
Multiparity is considered a risk factor for placenta praevia.
Increasing maternal age is a risk factor placenta praevia.
An ultrasonography of a 25 year old female at 24 weeks gestation reveals twin pregnancy.
Both foetuses are female and it appears to be a diamniotic, monochorionic twin pregnancy.
Twin A appears much smaller than Twin B.
Which of the following is a concern for Twin B?
What is the cause?
Hypervolaemia
The recipient twin would develop hypervolemia as a result of receiving transfusion from the donor twin (which would develop oligohydramnios and growth retardation).
You meet a 37-year-old woman on labour ward who is 40+5 weeks gestation and has elected to be induced.
You return shortly after induction to find the patient is barely responsive and visibly dyspnoeic.
Your colleage takes some observations which show the patient is hypoxic and hypotensive.
You suspect an amniotic fluid embolism.
Which of the following is the most appropriate next step in management?
Give the patient 15l oxygen via a non-rebreathe mask and call an anaesthetist
In amniotic fluid embolism, patients can quickly deteriorate and develop acute respiratory distress syndrome.
As such, the first step in management should be treating the maternal hypoxia in an effort to prevent any neurological sequelae
What is a sign of placental separation during the third stage of labour? (3)
Signs of placental separation and imminent placental delivery:
- Gush of blood
- Lengthening of the umbilical cord
- Ascension of the uterus in the abdomen
A 34 year women G3P2 is undergoing labour at 41 weeks gestation.
She has a history of two previous uncomplicated vaginal deliveries.
After 20 minutes of pushing, the midwife notices a visible umbilical cord in the vagina.
The patient is prepared for an emergency caesarean section.
What should the patient be instructed to do in the mean time?
Ask the patient to go on all fours, on knees and elbows
This is cord prolapse, which is an emergency as if left untreated because cord compression or spasm can lead to foetal hypoxia, irreversible damage, or death. As the patient is being prepared for an emergency caesarean section, they should be asked to on all fours on knees and elbows, while someone else pushes the presenting part of the foetus up to prevent cord compression.
You see a 25-year-old nulliparous patient in clinic who has recently had a singleton pregnancy confirmed.
She was diagnosed with epilepsy 6 years ago and has been seizure free for 18 months on her current dose of lamotrogine.
She is concerned about how her to manage both her epilepsy and pregnancy and is seeking advice.
She has no other medical history of note.
Which of the following is best advice to give this patient after delivering the baby?
It is recommended that she try to breastfeed after delivery
Anticonvulsant medication is present in breast milk in smaller quantities and allows the baby to withdraw slowly
A 35 year old primiparous woman attends antenatal clinic at 35 weeks gestation.
The baby has breech throughout the pregnancy and has failed to turn spontaneously.
She is thus offered an elective Caesarean section.
She is worried about the risks of having a Caesarean section, in particular the implications on any future pregnancies.
Regarding future placenta, which of the following statements is true after caesarean?
Increased risk of placenta accreta
Following Caesarean section there is increased risk of placental abnormalities for future pregnancies. Placenta accreta is the abnormal implantation of the placenta into the uterine wall, a common site being the old Caesarean scar.
A 22 year old woman presents to her GP at 34 weeks gestation with a new thick, white, odourless vaginal discharge.
She also complains her vulva is itchy and becoming red and sore.
She is otherwise well.
She has had no new sexual partners since becoming pregnant.
On examination, her blood pressure is 122/76, pulse 68, her abdomen is soft and non-tender with a fundal height appropriate for 34 weeks.
On external genital examination, the vulval area is red and excoriated.
There are no discrete ulcers or lesions. On speculum, there is copious thick lumpy discharge seen.
The cervix is long and closed. There is no bleeding seen.
What is the most likely diagnosis?
Vulvovaginal candidiasis
Vulvovaginal candidiasis (thrush) is common in pregnancy and typically presents with a thick white discharge (often described as ‘like cottage cheese’) which is usually odourless. It is a fungal infection that can cause itching and irritation around the vulva and vagina.
Candidiasis should be treated in pregnancy with an intravaginal antifungal agent such as a Clotrimazole pessary +/- a topical antifungal cream e.g. Clotrimazole. Oral antifungal medication is not recommended for pregnant women
A 24 year old woman presents to her GP at 30 weeks gestation suffering with ‘heartburn’.
She describes a retrosternal burning sensation, which commonly occurs following eating, or when lying in bed at night.
Which hormone is responsible for the promotion of smooth muscle relaxation, which contributes to reduced oesophageal tone and reflux oesophagitis?
Progesterone
Progesterone is increased throughout pregnancy.
It is produced by the corpus luteum in the first four weeks of pregnancy and by the placenta thereafter.
It promotes smooth muscle relaxation in the digestive system, urinary system and uterus.
A 25 year old primiparous woman presents to the day assessment unit at 37 weeks gestation with rupture of membranes.
This occurred 24 hours ago but still no contractions have occurred yet.
She feels generally well with no vaginal bleeding or pain.
A cardiotocograph is normal and the mother reports that the baby has been moving normally.
On examination her temperature is 36.8ºC, symphysis-fundal height is 34cm and the fetus is cephalic presentation with 3/5 palpable.
Which of the following is the next most appropriate step in her management?
She should be offered an induction of labour as it has now been 24 hours since the rupture of membranes with no commencement of labour.
This is the most appropriate answer. Following rupture of membranes if spontaneous labour does not occur within 24 hours induction of labour should be offered.
A 24-year-old lady attends a pre-conception clinic for advice.
She has a past medical history of epilepsy well controlled with Valproate.
Her doctor advises her that it is important to switch to a safer antiepileptic drug (AED) in pregnancy.
Which of the following is the most common fetal anomaly associated with Valproate?
Neural tube defects
This is the correct answer. Valproate exposure in the first trimester is associated with the highest risk of major congenital malformations. These include neural tube defects, cardiovascular anomalies, genital abnormalities, skeletal abnormalities and developmental delay. AEDs such as Valproate, Phenytoin and Carbamazapine are known to be associated with the risk of development of neural tube defects.
A 30 year old primiparous woman is inactive labour at 37 weeks gestation.
She is having a vaginal delivery and is currently in the second stage of labour.
She has been pushing regularly with contractions and the fetal head has now extended fully out of the vaginal introitus.
The fetal head is in an occipito-anterior position.
What is the next step in this labour?
Restitution
Following delivery of the fetal head, the fetus externally rotates (restitution) to bring the shoulders into an antero-posterior position. This facilitates delivery of the anterior shoulder and expulsion of the fetus.
What is restitution?
Restitution
Following delivery of the fetal head, the fetus externally rotates (restitution) to bring the shoulders into an antero-posterior position. This facilitates delivery of the anterior shoulder and expulsion of the fetus.

A 17-year-old woman presents to her GP.
She states that her menstrual period has been several weeks later than expected, which is unusual as her menstrual cycle is normally very regular.
She also explains that her period was accompanied by some “grey bits” and a few blood clots.
She had unprotected sexual intercourse with someone at a party 5 weeks ago.
Which of the following is the most likely diagnosis?
Miscarriage
If the woman had become pregnant because of her unprotected sexual intercourse this would explain why her period did not occur when she was expecting it.
Passage of fetal and placental tissue during a miscarriage can appear as greyish tissue and be accompanied by blood clots.
Indications for Category 1 Caesarean sections?
(2)
Category 1 (immediate) Caesarean section should be performed where there is evidence or clinical suspicion of acute foetal compromise:
- cord prolapse
- Scalp pH <7.2 is an indication for category 1 Caesarean section
A 14 year old female presents to her GP with a positive pregnancy test, nausea and slight vaginal bleeding.
She does not know when her last menstrual period was.
She is referred to the antenatal clinic where a a transvaginal ultrasound is performed.
The transvaginal ultrasound shows a ‘cloud like’ appearance and she is diagnosed with a molar pregnancy.
Which of the following is true regarding management of a molar pregnancy? (2)
The molar pregnancy requires removal as it is not viable. This is usually achieved surgically using a dilatation and curettage
Correct. A molar pregnancy (or hydatidform mole) occurs when there is an abnormality in the usual fusion of sperm and egg, resulting in a rapidly dividing tissue mass which is not compatible with a normal pregnancy.
Molar pregnancies can be subdivided into:
- Complete mole = Occurs when one or two sperm fertilise an egg that contains no chromosomal material. Therefore there is no maternal chromosomal material. A placenta is formed but there is no embryo.
- Partial mole = Occurs when two sperm fertilise a normal egg and instead of forming twins, there is an abnormal proliferation of tissue. There is embryonic tissue, but this is not a viable pregnancy.
A molar pregnancy is not a viable pregnancy and requires removal as there is a risk it may progress to invasive or malignant disease.
A 28 year old G2P2 is nearing term and has planned to breastfeed her baby after delivery.
She is wondering which of her medications is safe to continue during breastfeeding.
Which asthmatic drug is permitted during breastfeeding?
Which drugs are absolutely contra-indicated?
Salbutamol
The absolute contraindications to breastfeeding are:
- Infants of mothers with TB infection
- Infants of mothers with uncontrolled/unmonitored HIV
- Infants of mothers who are taking medications which may be harmful e.g. amiodarone
A 30-year-old, 41 week pregnant woman with gestational diabetes has failed to progress in the second stage of labour and is becoming distressed.
You suspect shoulder dystocia and call for additional help.
An episiotomy has been performed.
What of the following is the most appropriate next step in management?
McRoberts’ manoeuvre
After an episiotiomy has been performed, the patient should be placed in McRoberts’ position.
This involves hyperflexion at the hips with the thighs abducted and externally rotated
Gaskin manoeuvre
Gaskin manoeuvre
The Gaskin manoeuvre involves the patient rolling over to an ‘all fours’ position. The change in pelvic dimensions may assist with delivery
Rubin II manoeuvre
Rubin II manoeuvre
This is an internal manoeuvre used in shoulder dystocia involving applying external pressure to the posterior aspect of the anterior shoulder.
If successful, it allows the shoulders to be adducted and rotated to the larger oblique diameter