Final Test COPY Flashcards
(148 cards)
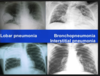
- Identify and discuss diagnostic considerations for evaluating pneumonia.*
- Differentiate between typical and atypical pneumonia
- Typical
- Generally Lobar pattern, classic presentation, “typical” pathogens
- Atypical
- Generally Interstitial pattern, atypical presentation, “atypical” pathogens (no growth on standard culture media, nothing seen on Gram’s stain), Viral

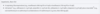
Contrast clinical findings in presentations of restrictive and obstructive lung processes.
- Does this describe obstructive or restrictive lung disease?
- Blue is normal
obstructive
Identify types of pneumoconiosis and the compounds that initiate disease.
Chest XR finding: Large masses of dense fibrosis in the UPPER zones
- State which pneumoconiosis is associated with the above Chest XR finding. Options are below
- Silicosis
- Coal workers’ pneumoconiosis
- Asbestosis

Identify types of pneumoconiosis and the compounds that initiate disease.
Chest XR finding: Large masses of dense fibrosis in the UPPER zones
- State which pneumoconiosis is associated with the above Chest XR finding. Options are below
- Silicosis
- Coal workers’ pneumoconiosis
- Asbestosis

- Recall and be able to perform the major components of the lung exam (inspection, palpation, percussion and auscultation).*
- What order do you perform a lung exam in?
Recall and be able to perform the major components of the lung exam (inspection, palpation, percussion and auscultation).
- What order do you perform a lung exam in?
-
Order Of Exam:
- 1. Look
- 2. Feel
- 3. Listen (Includes percuss)
-
Order Of Exam:
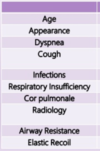
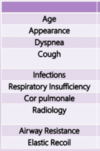
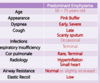
- Discuss the typical clinical presentation and diagnostic findings of chronic obstructive lung disease including emphysema and chronic bronchitis.*
- Describe COPD that is predominantly emphysema as it relates to everything listed
- Know examples of how pathogens can evade immune responses and define a successful pathogen*
- What are the 5 features of a successful pathogen?
Know examples of how pathogens can evade immune responses and define a successful pathogen
- What are the 5 features of a successful pathogen?
- Gains access to a host
- Finds a unique site (niche)
- Avoids host protective mechanisms
- Multiplies in host
- Often causes disease
Describe the composition, synthesis, mechanism of action and function of lung surfactant.
- What is the lipid and protein composition of surfactant?
- What is the predominant lipid?
- What cells secrete surfactant?
- Surfactant production in humans begins in Type II alveolar cells during the alveolar sac stage of lung development.
- Lamellar bodies appear in the cytoplasm at about 20 weeks gestation.
- These lamellar bodies are secreted by exocytosis into the surface water layer lining the alveolar airspace, where the surfactant forms a meshwork of tubular myelin.
-
Term infants are estimated to have an alveolar storage pool of approximately 100 mg/kg of surfactant, while preterm infants have an estimated 4–5 mg/kg at birth.
- Think IRDS

- Describe the changes in lung smooth muscle and cellular infiltrates associated with asthma.*
- What is shown in these pictures?


Discuss the pathophysiology, clinical presentation and treatment of bronchiolitis.
- What are the signs/symptoms of bronchiolitis?
- How do you Dx this?
- How do you treat this?
- What complications arise?
- How do you prevent bronchiolitis?
Discuss the pathophysiology, clinical presentation and treatment of bronchiolitis.
- What are the signs/symptoms of bronchiolitis?
- Low grade fever
- Irritability
- Increased work of breathing
- Very young infants may not have a prodrome, may have apnea as the first sign of infection
- Prolonged expiratory phase
- Nasal flaring
- Intercostal retractions (Sometimes)
- Suprasternal retractions (Sometimes)
- Air trapping with hyper-expansion of the lungs
- How do you Dx this?
- Laboratory studies are not required but quick test in office is easily done
- Pulse oximetry is adequate for monitoring oxygenation
- Frequent regular assessments of cardiorespiratory status is necessary
- Infants may develop respiratory failure quickly if they are very tired
- How do you treat this?
- Hospitalize if respiratory distress, hypoxia, under 4 months of age
-
Supportive care includes:
- Cool, humidified oxygen
- Nasopharyngeal suctioning
- Chest physiotherapy
- Elevate head of bed
- IV fluids if unable to take oral feeds
- What complications arise?
-
Short Term
- Dehydration (water loss due to increased respiratory rate)
- Acidosis
-
Late Term
- Asthma later in childhood
- Recurrence is common, tends to be mild, treatment same as the first episode
-
Short Term
- How do you prevent bronchiolitis?
- Palivizumab (RSV monoclonal antibody) Initiate just before onset of RSV season
- Monthly injections, 15mg/kg per dose
- Indicated for those under 2 years with chronic lung disease, very low birth weight, hemodynamically significant cyanotic and cyanotic heart disease
- Immunization with influenza vaccine over 6 months
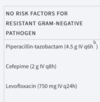
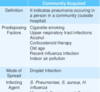
Differentiate between community-acquired and hospital-acquired bacterial pneumonia.
- Define HAP
- What are some predisposing factors to CAP?
- What are the common bacterial causes of CAP (differentiate between early onset and late onset)?
- What is VAP?
- VAP: Ventilator-Associated Pneumonia (≥ 48hrs after endotracheal intubation)

Differentiate between community-acquired and hospital-acquired bacterial pneumonias.
- HAP Tx
- If a patent has risk factors for MRSA, what do you do?

Differentiate between community-acquired and hospital-acquired bacterial pneumonias.
- Outpatient CAP Tx
- What can you give to a previously healthy patient who has not been on any antibiotics for the last 3 months?
3 options
- A macrolide
- Usually clarithromycin
- Azithromycin
- Doxycycline
Describe mutation analysis techniques and be able to recommend appropriate tests and interpret the results from that test.
- Do you need to know the mutation you are looking for with the following lab tests:
- • Sanger
- • PyroSequence
- • Next-Gen
- What is each test above used for and name an advantage or disadvantage for each?

Summarize the various presentations of different types of lung cancers.
- Malignant Mesothelioma
- Where do these arise in the body?
- How long is the latent period for this?
- What are the three morphologic appearances of this?
- What do signs/symptoms do patients present with?
- Is metastasis common?
- What is seen when the lungs are examined at autopsy?
- How does asbestos relate to smoking?
Summarize the various presentations of different types of lung cancers.
- Malignant Mesothelioma
- Where do these arise in the body?
- Usually in the parietal or visceral pleura
- It also occurs much less commonly in the peritoneum and pericardium.
- How long is the latent period for this?
- The latent period for developing malignant mesothelioma after the initial exposure is long, often 25 to 40 years.
- What are the three morphologic appearances of this?
-
Epithelial,
- Cuboidal cells with small papillary buds line tubular and microcystic spaces;
-
Sarcomatous
- Spindled, occasionally fibroblastic-appearing cells grow in sheets
-
Biphasic
- Both sarcomatous and epithelial areas.
-
Epithelial,
- What do signs/symptoms do patients present with?
- The presenting complaints are chest pain, dyspnea, and recurrent pleural effusions.
- Concurrent pulmonary asbestosis is present in only 20% of individuals.
- Is metastasis common?
- The lung is invaded directly, and there is often metastatic spread to the hilar lymph nodes and, eventually/rarely, to the liver and other distant organs.
- What is seen when the lungs are examined at autopsy?
- At autopsy, the affected lung typically is ensheathed by a layer of yellow-white, firm, variably gelatinous tumor that obliterates the pleural space.
- How does asbestos relate to smoking?
- Exposure to asbestos in nonsmokers increases the risk for developing lung cancer 5-fold, while in heavy smokers exposed to asbestos the risk is increased approximately 55-fold.
- Where do these arise in the body?
Identify types of pneumoconiosis and the compounds that initiate disease.
Chest XR finding: Multiple small nodules in the UPPER zones and Hilar “eggshell” calcifications
- State which pneumoconiosis is associated with the above Chest XR finding. Options are below
- Silicosis
- Coal workers’ pneumoconiosis
- Asbestosis

Identify types of pneumoconiosis and the compounds that initiate disease.
Chest XR finding: Multiple small nodules in the UPPER zones and Hilar “eggshell” calcifications
- State which pneumoconiosis is associated with the above Chest XR finding. Options are below
- Silicosis
- Coal workers’ pneumoconiosis
- Asbestosis
Explain the diagnostic strategies for pulmonary arterial hypertension (PAH) and sleep apnea (SA).
- What are the 5 classes of PAH?
- What is a Polysomnography?
- What does chronic hypoxemia cause?
- What are the classes of sleep apnea?
- Polysomnography, also called a sleep study,
- a test used to diagnose sleep disorders.
- Polysomnography records your brain waves, the oxygen level in your blood, heart rate and breathing, as well as eye and leg movements during the study.
- Chronic Hypoxemia can cause:
- ▸ Pulmonary vasoconstriction
- ▸ 2 ̊ polycythemia
- ▸ Systemic hypertension
- ▸ Cardiac arrhythmias
- ▸ Sudden death
- Sleep Apnea Classes
- Obstructive (OSA)
- Obese
- Hypoxic
- Hypercapneic
- Excess parapharyngeal tissue = adults who snore loudly
- Adenotonsillar hypertrophy = children who snore loudly
- Central
- Toxic (opiates/sedatives)
- Trauma/infection/stroke
- Advanced HF
- Obstructive (OSA)

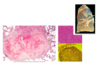
Identify types of pneumoconiosis and the compounds that initiate disease.
- What is notable about where asbestosis starts in the lungs?
- In asbestosis, contraction of the fibrous tissue distorts the normal architecture, creating enlarged air spaces enclosed within thick fibrous walls. What is the notable term used to describe the way the regions look?
- What is the most common manifestation of asbestos, and what are they made of /contain?
- What is shown in the image?
- How do patients with the asbestos present?
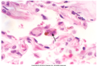
Identify types of pneumoconiosis and the compounds that initiate disease.
- What is notable about where asbestosis starts in the lungs?
- In contrast with CWP and silicosis, asbestosis begins in the lower lobes and subpleurally, spreading to the middle and upper lobes as the fibrosis progresses.
- In asbestosis, contraction of the fibrous tissue distorts the normal architecture, creating enlarged air spaces enclosed within thick fibrous walls. What is the notable term used to describe the way the regions look?
- Honeycombing
- What is the most common manifestation of asbestos, and what are they made of /contain?
- Pleural plaques are the most common manifestation of asbestos exposure and are well-circumscribed plaques of dense collagen, often containing calcium.
- They develop most frequently on the anterior and posterolateral aspects of the parietal pleura and over the domes of the diaphragm.
- What is shown in the image?
-
Asbestos bodies
- When asbestos fibers are inhaled, they become surrounded by alveolar macrophages and coated by a protein-iron complex, forming asbestos bodies.
- These bodies eventually undergo fibrosis, causing the lung tissue to become diffusely fibrotic and rigid and the airways to become distorted.
-
Asbestos bodies
- How do patients with the asbestos present?
- Progressively worsening dyspnea appears 10 to 20 years after exposure.
- It is usually accompanied by a cough and production of sputum.
- The disease may remain static or progress to CHF, cor pulmonale, and death.

Describe the differences between emphysema and bronchitis.
- Both emphysema and bronchitis present with SOB. What are the other 2 main presentations for bronchitis?
Describe the differences between emphysema and bronchitis.
- Both emphysema and bronchitis present with SOB. What are the other 2 main presentations for bronchitis?

Understand and be able to discuss common bacterial pathogens responsible for upper respiratory tract infections, including those that present as sinusitis, pharyngitis, epiglottitis.
- Group A (Streptococcus pyogenes)
- What can patients with a URI from this present with?
- List and describe the 3 conditions that can happen if this is untreated?
Understand and be able to discuss common bacterial pathogens responsible for upper respiratory tract infections, including those that present as sinusitis, pharyngitis, epiglottitis.
- Group A (Streptococcus pyogenes)
- What can patients with a URI from this present with?
- Intense acute pharyngitis
- Glomerulonephritis
- Tonsillitis
- Redness and edema of mucus membranes
- Purulent exudate
- List and describe the 3 conditions that can happen if this is untreated?
-
Scarlet fever
- - High fever > 38.30C
- Sandpaper rash
- Strawberry tongue
- Circumoral palor
-
Rheumatic fever and Rheumatic heart disease
- Antibodies to M protein and other cell wall components also bind human cardiac sarcolemma
-
Post-Strep Glomerulonephritis
- 1-5 weeks after acute pharyngitis or streptococcal skin infection
- Blood and protein in urine, edema, hypertension, renal insufficiency, oliguria
- Deposition of immune complexes in the kidneys
- Majority of patients recover but it can be fatal or develop into chronic disease in rare cases.
-
Scarlet fever
- What can patients with a URI from this present with?
Recall and be able to perform the major components of the lung exam (inspection, palpation, percussion and auscultation).
- Describe these lung sounds
- Tracheal
- Bronchial
- BC
- Vesicular
- Adventitious
Compare and contrast the causes of atopic (extrinsic) versus non-atopic (intrinsic) asthma.
- For Atopic
- How common is this?
- What type of hypersensitivity is this, and what Ig molecule is it associated with?
- When does it start in life?
- Does it have a genetic component?
- What often precedes asthma attacks?
- What will a skin test show?
Compare and contrast the causes of atopic (extrinsic) versus non-atopic (intrinsic) asthma.
- For Atopic
- How common is this?
- The most common form of asthma
- What type of hypersensitivity is this, and what Ig molecule is it associated with?
- A classic example of type I IgE–mediated hypersensitivity reaction.
- When does it start in life?
- Childhood
- Does it have a genetic component?
- Yes, a positive family history of atopy and/or asthma is common
- What often precedes asthma attacks?
- Allergic rhinitis, urticaria, or eczema.
- What will a skin test show?
- Wheal and Flare Rxn
- How common is this?
Understand and be able to discuss common bacterial pathogens responsible for upper respiratory tract infections, including those that present as sinusitis, pharyngitis, epiglottitis.
- Bordatella pertussis AKA Whooping Cough
- Describe the catarrhal stage
- Describe the paroxysmal stage
- When is the initiation of treatment pointless?
Understand and be able to discuss common bacterial pathogens responsible for upper respiratory tract infections, including those that present as sinusitis, pharyngitis, epiglottitis.
- Bordatella pertussis AKA Whooping Cough
- Describe the catarrhal stage
- 2 week incubation
- Mild disease if anything but highly infectious
- Describe the paroxysmal stage
- After two weeks.
- Explosive whooping cough
- Whoop upon inhalation leading to rapid exhaustion -
- Associated with vomiting, cyanosis, convulsions
- Dangerous complications in infants
- Rarely can lead to seizures and encephalopathy.
- When is the initiation of treatment pointless?
- Treatment initiated after the start of the paroxysmal stage rarely alters the clinical
- Describe the catarrhal stage
- Describe risk factors other than smoking that can lead to increased lung cancer risk.*
- What are the common occupational exposures that have an increased risk of lung cancer?
Describe risk factors other than smoking that can lead to increased lung cancer risk.
- What are the common occupational exposures that have an increased risk of lung cancer?
- Uranium Mines
- Work with asbestos
- Inhalation of dust containing arsenic, chromium, nickel, or vinyl chloride.
Describe pathophysiology of cystic fibrosis and how this relates to morbidity and mortality. Explain clinical presentation and diagnosis of cystic fibrosis.
- How do each of the following characteristics of CF present?
- Acute Pulmonary exacerbation
- Chronic Pulmonary Clinical Complications
- Exocrine Clinical complications
- GI Clinical complications
- Reproductive Clinical Complications
- Integumentary Clinical Complications
-
Acute Pulmonary exacerbation
- • Increase in cough
- • Fever
- • Change in sputum
- • Decreased activity, lethargy
- • Hemoptysis
-
Chronic Pulmonary Clinical Complications
- • Recurrent pulmonary infections
- • Sinusitis
- • Pneumonia
- • Bronchiectasis
-
Exocrine Clinical complications
- • Pancreatic insufficiency
- • Pancreatitis
- • Malabsorption of fat-soluble vitamins
- • 30% develop diabetes mellitus
- • Failure to thrive
-
GI Clinical complications
- • Meconium ileus in newborns
- • Malabsorption with steatorrhea of fat-soluble vitamins
- • Rectal prolapse
- • Prolonged neonatal jaundice
-
Reproductive Clinical Complications
- • 99% of males struggle with fertility
- • Increased difficulties with fertility for females
-
Integumentary Clinical Complications
- • “salty” skin
- • clubbing of fingers