Gargi & Emma's Notes - Obstetrics Flashcards
(446 cards)
When do most caeses of asthma in pregnancy occur?
Most occur between 24-36 weeks
What is asthma?
Chronic inflammatory airway disease characterized by:
- variable reversible airway obstruction,
- airway hyper-responsiveness
- bronchial inflammation
What are the clinical signs of asthma in pregnancy?
- Wheeze, breathlessness, cough – worse in morning and at night
- Precipitating factors – e.g. cold, drugs (beta blocker, NSAIDs), exercise
- Atopic history
- Tachypnoea, use of accessory muscles, prolonged expiratory phase, polyphonic wheeze, hyperinflated chest
What is classified as a severe attack of asthma in pregnancy?
Severe attack if PEFR <50%, pulse >110, RR > 25, inability to complete sentences
What is classified as a life-threatening attack of asthma in pregnancy?
Life-threatening if:
- confusion,
- coma
- cyanosis,
- PFR <33%,
- silent chest,
- bradycardia,
- hypotension,
What are the investigations for ?asthma in pregnancy?
- Chronic:
- PEFR monitoring
- Acute:
- Basic obs (incl pulse oximetry)
- PEFR
- pulse oximetry
- ABG, FBC, (WCC infection?), U&Es
- blood/sputum cultures
- CXR (exclude other diagnoses)
What is the antenatal management of chronic asthma?
Chronic management:
- Antenatal:
- MDT approach
- Reassurance that asthma medication is safe during pregnancy à continue taking as normal
- Oral corticosteroids have small increased risk of malformations
- Optimise control
- Smoking cessation
- NB stepwise approach is:
- Step 1: salbutamol PRN
- Step 2: add low-dose ICS (400mcg/day)
- Step 3: – + LABA/increase ICS to 800mcg/day
- Step 4: medium-dose ICS (2000mcg/day) + LABA (or theophylline or LTRA)
- Step 5: high-dose ICS + LABA/tiotropium
- Step 6: oral corticosteroid + high-dose ICS + LABA
NB safer to have medications than to have asthma symptoms during pregnancy
What is management of chronic asthma during labour?
- In labour:
- Continue regular medications
- Avoid bronchoconstrictors if severe asthma (e.g. ergometrine, prostaglandins)
- Ensure adequate hydration
- Regional anaesthesia favoured over GA (to decrease risk of bronchospasm)
What is management of acute asthma during pregnancy?
Acute management:
- As for non-pregnant individuals
- Monitor O2 sats, ABG and PEFR
- ABCDE approach, high-flow O2
- Nebulised salbutamol (5mg initially continuous, then 2-4hourly) +/- ipratropium (0.5mg QDS)
- IV hydrocortisone (100-200 IV) followed by oral prednisolone for 5-7d (40mg PO)
- If no improvement: IV magnesium sulphate, IV aminophylline or IV salbutamol
- Summon anaesthetic help if pt getting exhausted PCO2 increasing
- ICU admission and ventilation if severe
- Discharge when PEFR >75% of pts best, diurnal variation <25%, stable on discharge meds for 24h
What are the complications of asthma in pregnancy?
Foetal complications:
- Possible increased risk of FGR & foetal brain injury
- (due to prolonged maternal hypoxia)
- Preterm labour + birth
- Perinatal mortality
- Increased cleft lip risk
- (due to oral corticosteroids use in 1st trimester)
- Inheritance for foetus (6-30%)
What is the prognosis of asthma during pregnancy?
- Prognosis → Severity of asthma remains stable in one third, worsens in another third and improves in the last
- Well-controlled asthma has little effect on pregnancy outcome
What are the 4 hypertensive diseases in pregnancy
- Chronic hypertension
- Gestational hypertension
- Pre-eclampsia
- Eclampsia
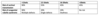
How is mild, moderate and severe HTN during pregnancy classified?
- Mild: 140-149 / 90-99
- Moderate: 150-159 / 100-109
- Severe: >=160 / >=110
Define chronic HTN in pregnancy.
Give some causes.
- Chronic hypertension: sustained BP readings ≥140/90 which occurred <20wks gestation or persists for >12wks postpartum
Essential in 90%, secondary in others
Endo – Cushing, pheo, CAH, Conn’s
Renal – RAS, chronic disease
Vasc – coarctation of aorta
RF – old age, ethnicity (Afro-Carib), obesity, smoking, diabetes, FHX, pre-eclampsia
# Define gestational HTN. Describe its aetiology.
- Gestational hypertension: sustained BP readings of ³140/90 after 20wks gestation in a previously normotensive patient, resolving by 12wks postpartum, in the absence of proteinuria
- Aetiology is unknown; may be due to upregulation of the RAAS without the drop in SVR to balance BP
What are the signs of chronic HTN in pregnancy?
Chronic –
- largely asymptomatic,
- BP may be normal in first trimester due to reduced systemic vascular resistance,
- secondary causes – renal bruits (RAS), radio-femoral delay (coarctation)
What are the Ix for ?chronic HTN in pregnancy?
- Bloods – FBC, UE, LFT, Urate, TFTs
- Urinalysis – proteinuria, catecholamines
- Renal artery USS
- Foetus – serial USS for growth
What is the Mx of chronic HTN prior to pregnancy?
- medication changed to non-teratogenic ie methyldopa, nifedipine, labetalol (NOT ACEi/ARBs),
- (increased risk of congenital abnormality/neonatal complications)
- May need reduced doses of other antihypertensives in the first half of pregnancy (when BP drops)
- Lifestyle advice
- Aim to keep BP <150/100
- aspirin 75mg of to reduce pre-eclampsia risk/IUGR.
- Monitor for pre-eclampsia, serial USS for growth, uterine artery Dopplers at 24/40 for risk
What is the Mx of mild chronic/gestational HTN in pregnancy?
- Lifestyle modification
- Consultation with dietitian; aim for limited/no weight gain in obese patients, reduce salt etc.
- Monitor BP around 1/wk to detect changes and signs of pre-eclampsia
What is the Mx of moderate chronic/gestational HTN in pregnancy?
- Lifestyle modification
- Antihypertensives
- Oral labetalol (1st line) à aim for <150/80-100; avoid labetalol in asthma
- Alternatives are methyldopa and nifedipine
- Close monitoring of BP and signs of pre-eclampsia (2x/wk); monitor for FGR
- Aim for delivery >37wks; may be earlier if complications (e.g. IUGR, development of pre-eclampsia)
What is the Mx of severe chronic/gestational HTN in pregnancy?
- Admit to hospital (until BP is <160/110)
- Antihypertensives
- IV labetalol or IV hydralazine
- Convert to oral labetalol/methyldopa when BP is under control
- BP monitoring at least 4x/d; daily urine monitoring for protein, monitor for FGR
- Consider delivery if severe refractory gestational HTN or >37wks
What is the Mx of severe chronic/gestational HTN post-natally?
- In gestational HTN, measure BP daily for 2 days, and at least once between day 3 and 5
- Reduce antihypertensives as their BP falls
- If BP remains high 6-8wks after birth à medical review
What is the prognosis of chronic HTN?
- Maternal risks: pre-eclampsia, abruption, HF, intracerebral haemorrhage
- Pre-eclampsia develops in 1/3
- –> RFs for developing superimposed pre-eclampsia are:
- renal disease,
- maternal age >40yo,
- pre-existing DM,
- multiple pregnancy,
- connective tissue disease (antiphospholipid),
- coarctation of aorta,
- severe HTN,
- BMI >35,
- previous pre-eclampsia
What are the complications of pre-eclampsia?
- Maternal – eclampsia, abruption, CVA, pulmonary oedema, cerebral oedema, renal/liver failure, DIC, HELLP syndrome (haemolysis, elevated liver enzymes, low platelets)
- Foetal – IUGR, death