Histo: Bone Pathology Flashcards
(70 cards)
What are the main functions of bone?
- Mechanical - support and site for muscle attachment
- Protective - vital organs and bone marrow
- Metabolic - store of calcium
Outline the composition of bone.
- Inorganic (65%) - calcium hydroxyapatite, storehouse of 99% of body calcium (and 85% of phosphorus, 65% of sodium and magnesium)
- Organic (35%) - bone cells and protein matrix
In which part of a bone is the growth plate found?
Metaphysis

What are the main features of cortical bones?
- Long bones
- 80% of skeleton
- Appendicular
- 80-90% calcified
- Mainly mechanical and protective
What are the main features of cancellous bones?
- Vertebrae and pelvis
- 20% of skeleton
- Mainly axial
- 15-25% calcified
- Mainly metabolic
- Large surface
Describe the microanatomy of bone.
- Made up of several micro-columns
- Haversian canals are found at the middle of the micro-columns
- Volkmann canals are canals that connect the Haversian canals
- Around the Haversian canals are concentric lamellae and in between these units will be interstitial lamellae
- Around the entire bone you will find circuferential lamellae
- In the middle the bone will be trabecular lamellae

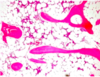
Describe the histological appearance of cancellous bone.
Trabeculae are dark pink areas and in between you will find adipose tissue with haemopoietic cells
What are the three main types of bone cell and what are their roles?
- Osteoblasts - build bone by laying down osteoid
- Osteoclasts - multinucleate cells of the macrophage family that resorb bone
- Osteocytes - osteoblasts-like cells that sit in the lacunae

Which protein is important in regulating the action of osteoclasts?
Osteoblasts produce osteoprotegrin which blocks the RANK-RANKL interaction which prevents the differentiation of an osteoclast precursor into a fully functioning osteoclast

Define metabolic bone disease.
A group of diseases characterised by disordered bone turnover due to imbalance of various body chemicals.
NOTE: overall effect tends to be osteopaenia
What are the three main categories of metabolic bone disease?
- Non-endocrine (e.g. age-related)
- Endocrine (e.g. vitamin D, PTH)
- Disuse osteopaenia
Where is bone usually sampled from for histological analysis of bone in metabolic bone disease?
Iliac crest
NOTE: the sample be processed and un-decalcified for histomorphometry
Which static parameters are measured in the histological analysis of bone in metabolic bone disease?
- Cortical thickness
- Trabecular bone volume
- Thickness, number and separation of trabeculae
Which technique is used to measure histodynamic parameters when investigating metabolic bone disease?
Tetracycline labelling
What are the most common causes of osteoporosis?
90% are due to insufficient calcium intake or post-menopausal oestrogen deficiency
List some primary and secondary causes of osteoporosis.
- Primary - age, post-menopause
- Secondary - steroids, systemic disease
Broadly speaking, what are the two rutes by which disordered bone turnover can cause osteoporosis?
- High turnover results in high bone resorption
- Low turnover results in low bone formation
- Both resulted in reduced bone mass
What are the effects of long-term steroid use on bone?
- Affects all three bone cell types
- Leads to decrease in bone quality
- Ultimately results in osteonecrosis and fracture
Describe the ways in which osteoporosis can present.
- Back pain
- Pathological fractures
- Wrist (Colles’)
- Hip (NOF, intertrochanteric)
- Pelvic
- Vertebra (60% asymptomatic)
Which investigations may be used in a patient with suspected osteoporosis?
- Serum calcium, phosphate and ALP (should be NORMAL)
- Urinary calcium
- Collagen breakdown products
- Imaging
- DEXA
Which four organs are affected by PTH and have a role in calcium homeostasis?
- Kidney
- Bone
- Proximal small intestine
- Parathyroid gland
Define osteomalacia.
Defective bone mineralisation
What two underlying abnormalities can cause osteomalacia?
- Deficiency of vitamin D
- Deficiency of phosphate
What is the main histological feature of osteomalacia?
Reduced amount of mineralised bone compared to the amount of osteoid













