GI Path Flashcards
Which has better prognosis: pedunculated or sessile polyps?
Pedunculated– easier to resect
What is the MCC of pseudopolyps in the colon?

Ulcerative colitis
Juvenile polyps: benign or malignant
Rarely malignant; can rarely get Polyposis Syndrome
ID

Peutz-Jeghers Syndrome: hyperpigmentation @ lips/gingiva + harmatomatous polys (benign)
Have increased risk of cancer, but not from polyps themselves
Colonic Hyperplastic Polyps:
- Common or rare?
- Benign or malignant?

Common
Benign but MUST be distinguished from Sessile Serrated Adenomas
When might you suspect Colonic Hyperplastic Polyps may actually be Sessile Serrated Adenomas?

Large (>1cm) in RIGHT colon
– DNA mismatch repair pathway affected
Adenoma of Colon:
- common or rare?
- Benign or malignant?
- Common
- ALWAYS have dysplasia – ALWAYS pre-malignant
Most colon cancers arise from what?
Adenoma of colon- always pre-malignant, but good to find because they can be removed before they become malignant
How can you tell if Adenoma of Colon has invaded?

Stromal desmoplasia
Familial Adenomatous Polyposis

- Rare APC gene mutation
- 100% develop colon cancer
- Wall-to-wall adenomas = FAP until proven otherwise
Main risk factor for Colon Cancer besides genetics?
Diet– better to eat high fiber & fruits & veg
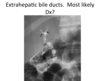
Dirty necrosis

Probably coming from colon
Mucin all up in that peritoneal cavity…

Check appendix!
Yellow tumor in small intestine

Carcinoid
Carcinoid syndrome:

HTN, flushing, diarrhea
MC metastatic site = liver (CT scan)
GIST: prognosis based on? diagnosis?
Prognosis based on size & mitotic rate
CD-117 stain helps confirm dx & prognosis
Appendiceal carcinoids: location? common? prognosis?

@ tip usually
Common
Good prognosis
Appendiceal Mucinous Cystadenocarcinoma: morphology

- Mucin + epithelial cells in peritoneal wall
- Pseudomyxoma peritonei (lots of mucin in peritoneal cavity)
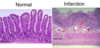
ID

Tubulovillous Adenoma
(Intestinal adenomas can be Tubular, Villous, or Tubulovillous)
Morphology of Esophagus with Achalasia
Loss of inhibitory neurons in wall of intestine (enteric)
How are esophageal webs & rings formed?
Post-inflammational scarring (most common)
Tumors
What is the cause of diverticuli?

Esophageal spasms
What is the cause of Mallory-Weiss syndrome?

Persistent vomiting (alcoholics, eating disorder)
Usually not too severe
Cause of Esophageal Varices? Severity?

Portal HTN (from cirrhosis)
Can rupture– 50% mortality :(