Head and spinal injury Flashcards
(75 cards)
Which type of head injury is most common?
Blunt trauma (as opposed to penetrating)
Common causes of head injury
- RTAs
- Falls
- Assaults
- Sports
- Workplace injuries
Primary vs secondary brain injury
Primary: occurs at time of injury, axonal shearing and disrutpion with associated areas of haemorrhage
Widespread: diffuse axonal injury
Localised injury: coup-contre-coup
>>The only cure for this would be to prevent accidents/ damage limitation e.g. helmets<<
Secondary: occurs later, due to various problems that commonly occur e.g. hypoxia, hypovolemia, intracranial haematoma and raised ICP, epileptic fits, infection
>>The aim of managament in ED is to prevent secondary traumatic brain injury<<
How do we calculate CPP?
MAP - ICP
MAP = systolic BP + diastolic BP + diastolic BP
Following head injury, what are the indications for referral to hospital?
- Impaired consciousness at any time
- Amnesia
- Neuro symptoms: vomiting, severe headache, seizures
- Skull fracture: CSF leak, peri-orbital haematoma
- Significant extracranial injuries
- Worrying mechanism e.g. high energy/ NAI
- Comorbidity e.g. anticoagulant use/ alcohol
- Adverse social factors e.g. home alone
Simple method of assessing the severity of a head injury
AVPU
Patient unresponsive/ only responding to pain - call for senior help + ICU/ anaesthetist as patient will need expert airway care and IPPV
Monitoring of patients following head injury
Every head-injured patient must receive regularneurological obs - early identification of complications e.g. intracranial haematoma, fits and hypovolaemia is esstntial in order for early treatment
Any deterioration in GCS is an emergency - re-examine and correct problems + call for senior help
Important to know about when taking a head injury hx
Mechanism: allows for impression of the forces involved and risk of complications
Time of injury
Loss of consciousness/ amnesia: unconsciousness suggests at least moderate severity, 30mins+ amnesia warrants head CT
Subsequent symptoms: headache, N&V, weakness, sensory loss, visual disturbance, rhinorrhoea, otorrhoea
PMHx: anything that could have caused the injury/ make it worse e.g. epilepsy, cardiac arrhythmias, DM, coagulopathy, thrombocytopenic
Drug hx: drugs/ alcohol, antigoagulants, patients on clopidogrel may be at higher risk of intracranial haemorrhage following head injury so low CT threshold
Social: is there someone at home/ someone they can stay the night with
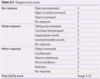
Discuss the GCS score
Scored from 3-15 assessing eye response, verbal response and motor response
Unconsciousness is taken to mean no eye response and GCS =<8
Simple blood test essential in all patients presenting to a&e following head injury/ confused
BLOOD GLUCOSE
DONT EVER FORGET GLUCOSE
Areas to cover in examination following head injury
C-spine
GCS
Vital signs/ obs
Blood glucose
Alcohol: never assume low GCS is due to alcohol
Eye signs: pupils
Scalp, face, head: cranial nerves
Limbs: neuro exam
Other injuries: intra-abdominal injuries often co-exist with serious head injuries
Signs of base of skull fracture
Often a clinical diagnosis
- Bilateral orbital bruising confined to orbital margin: panda eyes
- Subconjunctival haemorrhage
- Bleeding from ears/ blood behind typanum
- CSF otorrhoea and rhinorrhoea: separates into double ring when dropped on blotting paper
- Battle’s sign: brusing behind ears without local direct trauma - occurs due topetrous temporal bone facture - takes a few days to appear

Clinical features pointing towards an intracranial haematoma
Emergence of focal neurological signs
Deteriorating GCS
Indications for CT scan following head injury
GCS <13 on initial assessment
GCS <15 after 2hrs
Suspected skull fracture/ basal skull fracture
Post injury seizure
Focal neurological deficit Vomiting
Amnesia >30mins
LOC
Dangerous mechanism
Most requests will be urgent - scan interpreted within 1hr
Initial management of a head injury
ABCDE dont ever forget GLUCOSE
2x IV large bore cannula
Bloods: FBC, clotting screen, U&E, glucose
If GCS =<8: rapid sequence induction + intubation
Arrange CT
Give IV antibiotics for compound skull fracture
Liaise w/neurosurgery early
Urinary catheter
Treating complications of head injury
Diminishing consciousness likely to reflect intracranial pathology leading to rise in ICP
Liaise w/ neurosurgeon: they may advise use of mannitol to decrease ICP as a time buying measure
Hypertonic saline acts as an osmotic agent and can dcrease ICP whilst increasing intravascular volume
What medical therapy is used to reduce ICP to buy time?
Mannitol - bolus IV
Hypertonic saline
Investigations and management of patient with seizure
Check glucose and ABG
Give IV lorazepam - repeat once if it doesn’t work
IVI phenytoin with ECG monitoring (can cause bradycardia when given IV)
Levetiracetam is an alternative to phenytoin
Seizure >10-15mins - senior help, RSI, intubation and IPPV
Golden rules for managing head injury
- Never attribute low GCS to alcohol alone
- Never discharge a head-injured patient to go home alone
- Consider admitting patients with head injury who have a coagulopathy/ anticoagulants
Head injury warning instructions
Adults
- Ensure eye is kept on patient for 24hrs
- Rest 24hr
- Pain killers
- No alcohol for 24hrs
- Do not take sleeping tablets
- Any of the following, come back: persistent headache, vomiting, visual changes, balance problems, fits, unrousable
Children
- Child may be more tired than usual
- Allow them to sleep
- Pain killers
- Any of the following come back: persistent headache, vomiting, visual changes, balance problems, fits, unrousable
Post-concussion symptoms
Frequent: headache, dizziness, lethargy, depression, inability to concentrate
~30% patients have headaches for 2months
Migraine may become more frequent after head injury
Diagnosis of exclusion
Subdural haematoma: consider in alcoholics/ elderly and those on anticoagulants - low threshold for CT
How are post concussion symptoms managed?
Reassure + explain that they are likely to resolve gradually
Arrange appropriate follow up with GP
Concussion advice for those who play sport and high-level sport
Rest initially, especially when symptomatic
Take advice from those within their sport about when it is safe to return
Pulsatile tinnitus/ whooshing sound in one ear following head injury
Consider carotid/ vertebral artery dissection














