Hemodynamics Flashcards
(25 cards)
What factors affect the distribution of blood flow (cardiac output)?
- resistance: greater resistance will impede the distribution of blood flow
- pressure: blood moves from high to low pressure
- heart rate
- stroke volume
What is blood pressure?
- pressure exerted on the walls of a vessel
- generated by ventricular contraction
- presence of water in blood puts outward stretch on arteries
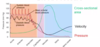
How does blood pressure change during the cardiac cycle?
- blood pressure is highest in the aorta
- diastolic and systolic pressures vary from 80-120mmHg
- pressure waves dampen as you move towards capillary system
- as you get further from the left ventricle, pressure drops
- pressure is almost 0 when entering the right atrium
- pressure is about 35mmHg entering the capillaries
- with decrease in blood volume over 10% BP drops
- water retention increases BP

How do cross sectional area and velocity of blood movement relate?
- as you move away from LV, cross sectional area increases as more branches, etc. of the vasculature occur
- speed of blood movement decreases with increased cross sectional area
- slow movement in the capillaries to allow for gas exchange
What are the systolic, diastolic, pulse, and mean pressures?
- systolic: highest pressure, ventricular systole
- diastolic: related to ventricular diastole
- pulse pressure: difference between systolic and diastolic, is a good indicator of CV health, small changes in systolic and diastolic pressures can increase pulse pressure
- mean arterial pressure: want to maintain this pressure, average pressure during entire cardiac cycle
What are Korotkoff sounds?
- when taking a blood pressure, cuff compresses brahcial artery
- when cuff is released, Korotkoff sounds are produced from the initial blood coming back into the artery
- this is measured as systolic pressure
- more blood will flow through and flow will become laminar
- when sounds are no longer heard, that is measured as diastolic pressure
What are pulse points?
- areas where we can compress the vessel against a bone or another structure
- dorsalis pedis often checked during surgery to make sure there is adequate perfusion to lower extremities

What equation represents mean arterial pressure?
-mean ABP= diastolic pressure +1/3 pulse pressure
or
-mean ABP= cardiac output x total peripheral resistance

What factors affect blood pressure?
- cardiac output (HR, SV)
- blood volume (blood loss- affects cardiac output and BP because this decreases venous return which affects afterload/preload, water retention)
- peripheral vascular resistance
What is an equation representing peripheral vascular resistance?
- pressure=flow x resistance
- flow=pressure/resistance
What is vascular resistance?
- blood close to wall of vessel causes friction
- friction can be influenced by blood vessel radius, blood viscosity, blood vessel length
- smaller vessel=increase in vascular resistance
- blood viscosity dependent on % of RBCs and lower water volume
- increase in viscosity=increase in resistance
- increase in BV length=increase in resistance
- arterioles control BP by changing diameter
- systemic vascular resistance aka total peripheral resistance
What factors can increase BP?

How is BP regulated?
Short term:
- neural: baroreceptor reflexes, chemoreceptor reflexes located in internal carotid arteries in carotid sinus/carotid bodies and aortic arch
- hormonal: EP, NE, ADH, ANP (atrial natriuretic peptide), renin-angiotensin-aldosterone system (longer term)
Describe the chemoreceptor/baroreceptor reflexes
- measuring changes in chemistry of blood (eg. oxygen, CO2, acidotic)
- stimulates cardiovascular centre to increase sympathetic stimulation which increases vasoconstriction and BP
- baroreceptors get stretched with increase in pressure which then signal through CNs to medulla oblongata (carotid signals through CN9, aorta signal goes through CN10)
- stimulates parasympathetics to decrease BP

Describe baroreceptor reflex for low blood pressure

What is orthostatic hypotension?
- fainting (syncope) when standing quickly
- baroreceptors work slower in the elderly or others where this might be a problem
Describe the baroreceptor reflex to an increase in BP

Describe short term hormonal regulation of BP
- with sympathetic stimulation, nerve impulses fire and get stimulation of adrenal glands
- increase of EP and NE in blood
- increase HR and force of contraction
- vasoconstriction doesn’t happen everywhere; may occur in skin and abdominal region
- may still have vasodilation in cardiac and skeletal tissue
Describe long term hormonal regulation of BP
- ADH (vasopressin): released from posterior pituitary, released in response to dehydration/decrease in blood volume, increases renal water retention and systemic vasoconstriction ->increases BP
- ANP: released by cells in atria, causes vasodilation, promotes renal loss of salt and water, lowers BP
- RAA system:

Michael was in a car accident and sustained a severe injury to his left leg. While waiting for the paramedics to arrive he lost a lot of blood. Paramedics noted: rapid resting heart rate, weak pulse, cool/clammy skin, sweating. What is the diagnosis?
-hypovolemic shock
- sympathetic stimulation causes increase in HR
- blood loss causes decrease in venous return and increase in HR causes short filling time leading to a decrease in end diastolic volume–> weak pulse
-cool/clammy skin: vasoconstriction of vessels towards skin, clamminess is from sweat glands
What is shock?
- failure of CV system to deliver enough O2 and nutrients
- inadequate perfusion
- cells forced to switch to anaerobic respiration
- lactic acid builds up
- cells and tissues become damaged and die
- system is designed to maintain mean arteriole BP
- compensation mechanisms: activation of RAA, secrete antidiuretic hormone, activate sympathetic nervous system, release of local vasodilators

What can occur from left sided heart failure? Right sided heart failure?
- left side of heart can’t function properly
- can get fluid accumulation in the lungs
- right sided: accumulation in feet

What is blood flow?
- volume of blood that flows through any tissue in a given period of time (mL/min)
- CO=HRx SV (total blood flow)
Consider the baroreceptor reflex. Which of the following will increase in response to a rise in arterial blood pressure?
a) parasympathetic activity to the heart
b) cardiac output
c) vasoconstriction of blood vessels
d) heart rate
e) adrenal secretion of EP
a) parasympathetic activity to the heart


