Inflammation, ischaemia, normal and abnormal development Flashcards
(111 cards)
What is inflammation?
A reaction to injury or infection involving cells such as neutrophils and macrophages.
When is inflammation good?
Infection or injury.
When is inflammation bad?
Autoimmunity or when an over-reaction to a stimulus.
How is inflammation classified?
Acute and Chronic.
What happens in acute inflammation?
Sudden onset
Short duration
Usually resolves
What are the steps in acute inflammation?
Initial reaction of tissue to injury
Vascular component: dilatation of vessels
Exudative component: vascular leakage of protein-rich fluid
Neutrophil polymorph is the characteristic cell recruited to the tissue
Outcome may be resolution, suppuration (e.g. abscess), organisation, or progression to chronic inflammation
What are the causes of acute inflammation?
Microbial infections, e.g. pyogenic bacteria, viruses
Hypersensitivity reactions, e.g. parasites, tubercle bacilli
Physical agents, e.g. trauma, ionising radiation, heat, cold
Chemicals, e.g. corrosives, acids, alkalis, reducing agents,
Bacterial toxins
Tissue necrosis, e.g. ischaemic infarction
What are the essential characteristics of acute inflammation?
Rubor (red due to blood vessels)
Calor (heat due to blood vessels)
Tumor (swelling due to oedema)
Dolor (Pain due to sweeling and stretching, bradykinin, prostaglandin and serotonin also cause pain)
Loss of function is also characteristic.
What happens in chronic inflammation?
Slow onset or sequel to acute
Long duration
May never resolve
What cells are involved in inflammation?
Neutrophil polymorphs
Macrophages
Lymphocytes
Endothelial cells
Fibroblasts
Plasma cells
What are neutrophil polymorphs and what are their function?
Short lived cells
First on the scene of acute inflammation
Cytoplasmic granules full of enzymes that kill bacteria
Usually die at the scene of inflammation
Release chemicals that attract other inflammatory cells such as macrophages
What are macrophages and what are their fuction?
Long lived cells (weeks to months)
Phagocytic properties
Ingest bacteria and debris
May carry debris away
May present antigen to lymphocytes
What are lymphocytes and what are their function?
Long lived cells (years)
Produce chemicals which attract in other inflammatory cells
Immunological memory for past infections and antigens
What are endothelial cells and what happens to them in inflammation?
Line capillary blood vessels in areas of inflammation
Become sticky in areas of inflammation so inflammatory cells adhere to them
Become porous to allow inflammatory cells to pass into tissues
Grow into areas of damage to form new capillary vessels
What are fibroblasts?
Long lived cells
Form collagen in areas of chronic inflammation and repair
What is an example of acute inflammation?
Acute pancreatitis
Empyema of the gall bladder
Fibrinous pleuricy
What is involved with acute pancreatitis?
Unknown precipitating factor
Neutrophils appear
Blood vessels dilate
Inflammation of serosal surface occurs
Pain felt
Appendix either surgically removed or inflammation resolves or appendix bursts with generalised peritonitis and possible death
What is an example of chronic inflammation?
Tuberculosis
What is involved with tuberculosis?
No initial acute inflammation
Mycobacteria ingested by macrophages
Macrophages often fail to kill the mycobacteria
Lymphocytes appear Macrophages appear Fibrosis occurs
What is the difference between an exudate and a transudate?
Exudates have a high protein content due to increased vascular permeability whilst transudates have a low protein content due to a normal vascular permeability.
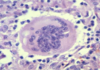
What is a granuloma?
An aggregate of epithelioiod histiocytes and a feature of some-specific chronic inflammatory disorders.
What is granulation tissue?
Granulation is an important component of healing and comprises small blood vessels in a connective matrix with myofibroblasts (A myofibroblast is a cell that is in between a fibroblast and a smooth muscle cell in phenotype)
What are histiocytes?
Specialised macrophages e.g. Kupffer cells
What is fibrin?
Deposited in blood vessels and tissues or on surfaces as a result of the action of thrombin or fibrinogen.