Pharmocology Flashcards
(218 cards)
WHAT IS PHARMOKINETICS?
The action of drugs in the body including/What the body does to a drug
ABSORPTION
DISTRIBUTION
METABOLISM
EXCRETION
What is absorption?
The process of transfer from the site of administration into the general or systemic circulation
What are some routes of administration of drugs?
Enteral (oral)
Enteric-coated (intestinal absorption, e.g. aspirin)
Extended-release (slower absorption, e.g. metformin)
Sublingual/Buccal (rapid absorption + avoids 1stpass metabolism)
Parenteral (systemic circulation)
Intravenous
Intramuscular (anti-psychotics)
Subcutaneous (insulin)
Other
Inhalation(oral, nasal)
Topical
Rectal
How many membranes must most drugs cross? What is the exception to this?
One. IV and IA.
How can transfer through a membrane occur?
Passive diffusion
Facilitated diffusion
Active transport
Endocytosis
What do drugs need to be to pass directly through the cell membrane?
Lipid soluble.
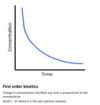
What is the rate of diffusion proportional to?
Rate of diffusion proportional to concentration gradient, the area & permeability of the membrane and inversely proportional to thickness.
What is drug ionisation?
Basic property of weak acids or weak bases.
Why are ionisable groups important for drugs?
The ionic forces are part of the ligand receptor interaction.
What is the PKa of a drug?
pH of which half the substance is ionised and half not.
Where are weak acids absorbed?
Stomach.
Where are weak bases absorbed?
Intestine.
What determines absorption of drugs?
pH
Vascularity (e.g. shock reduces SC absorption)
Surface area
Contact time (e.g. with food = slower gastric emptying)
What are four factors that determine the rate of absorption of an oral drug?
Drug Structure.
Drug formulation.
Gastric emptying.
First pass metabolism.
What do drugs need to be to be absorbed from gut?
Drug needs to be lipid soluble to be absorbed from the gut.
What happens with highly polarised drugs in the gut?
Highly polarised drugs tend to be only partially absorbed with much passed into the faeces.
Some drugs are unstable at low pH or in the presence of digestive enzymes.
What must a tablet be to be absorbed?
The capsule or tablet must disintegrate & dissolve to be absorbed.
Most do so rapidly. Some having coating e.g. Enteric.
What is first pass metabolism?
Concentration of a drug is greatly reduced before it reaches the systemic circulation
What major metabolic barriers do drugs have to cross to reach the circulation?
Intestinal lumen
Intestinal wall
Liver
Lungs
What is contained within the intestinal lumen which limits absorption?
Contains digestive enzymes that can split peptide ,ester & glycosidic bonds.
Peptide drugs broken down by proteases (Insulin).
Colonic bacteria hydrolysis & reduction of drugs.
What is contained within the intestinal wall which limits absorption?
Walls of upper intestine rich in cellular enzymes e.g. Mono amine oxidases (MAO)
Luminal membrane of enterocytes contains efflux transporters such as P-gp which may limit absorption by transporting drug back into the gut lumen
Extensive bowel surgery “short gut syndrome” – poor oral absorption as little surface left and rapid transit time.
How is the liver a metabolic barrier? How can you avoid this barrier?
Blood form gut delivered by splanchnic circulation directly to liver.
Liver is major site of drug metabolism
Avoid hepatic first pass metabolism by giving drug to region of gut not drained by splanchnic e.g mouth or rectum ( GTN )
WHAT IS DISTRUBITION?
Rate & extent of movement of a drug into (and out)of tissues from blood.
What factors control distrubition?
Blood flow (e.g. brain > muscles)
Capillary permeability
Plasma protein binding (e.g. albumin)
Tissue protein binding (e.g. cyclophosphamide accumulating in bladder leading to cystitis)
Lipophilicity(ability to cross cell membranes)