Lipids and Metabolism COPY Flashcards
(26 cards)
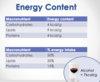
What is the energy content per gram of carbohydrates, lipids and proteins?
What proportion of our energy intake do the various macronutrients make up?
Proteins: 4kcal/g
Lipids: 9kcal/g
Carbohydrates: 4kcal/g
Carbohydrates make up 50% of energy intake
Lipids 35%
Proteins 15%
How is energy released from organic molecules?
Oxidation reactions - can involve adding of oxygen atoms but isnt always the case - oxidation is the loss of electrons
(opposite of oxidation is reduction, which is the gain of electrons). Oxidation applies to non organic molecules (Fe3+ more oxidised than Fe2+).
(For organic molecules, the more carbon/hydrogen and less oxygen they contain, the more scope there is for oxidising them)
Why do lipids contain more energy?
They are oxygen poor and hydrogen and carbon rich
What are the types of fatty acid based off length?
What constitutes an ‘unsaturated’ fatty acid?
What is the significance of this?
What is the significance of saturated fatty acids?
Fatty acids can be various lengths - considered long chain over 12 carbosn and very long chain over 22 carbons. Can be saturated or unsaturated.
Unsaturated –> Contains at least 1 double bond, meaning they contain less hydrogens. There is no rotation around the double bond, meaning they have fixed configuration at each double bond.
Double bond provides rigidity to the fatty acid- e.g. provides more rigidity to a cell membrane.
Saturated fatty acids contain more energy per gram
What is meant by ‘trans’ and ‘cis’ configurations?
Trans configurations: carbon chain crosses the double bond
Cis configurations: carbon chain kinks back on itself
What does the ‘omega’ nomenclature describe?
Other nomenclature?
Omega nomenclature –> describes the position of the final double bond, counting from the hydrocarbon end. e.g. Omega 9 fatty acid, double bond at 9th carbon from hydrocarbon end.
Other nomenclature uses C#1 : C#2 (triangle #, #) - where 1 is the number of carbons in chain, 2 is the number of double bonds, numbers in brackets are the positions of the double bonds.
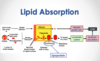
How are short chain fatty acids absorbed?
Simple diffusion across brush border of cell membrane and diffusion across basolateral membrane into blood. (carried into hepatic portal vein to liver).
How are long chain fatty acids absorbed?
Fats (triglycerides) emulsified by bile salts and phospholipids into emulsion droplets.
Digested by pancreatic lipase to monoglycerides and fatty acids.
Held in micelles, combined with bile salts and phospholipids.
Micelles diffuse into an ‘unstirred layer’ next to the surface of epithelial cells.
Monoglycerides and fatty acids diffuse into cell membrane.
Inside the cell monoglycerides and fatty acids are reassembled into triglycerides and packaged into chylomicrons
Exported across the basolateral membrane and leave the intestinal villus via the lacteals of its lymph system and into the systemic circulation.
Lymph re-joins the systemic circulation and gets carried to the liver
How are lipids transported through the blood plasma?
Describe the structure of a lipoprotein
Lipids are transported through aqueous blood plasma in structures called lipoproteins.
Lipoproteins have a hydrophobic core containing triglycerides and cholesterol esters and a hydrophilic surface containing phopsholipids, free cholesterol and proteins (apolipoproteins).

What releases fatty acids from chylomicrons and VLDLs into the tissues?
How can lipoproteins be separated into different classes?
Lipoprotein lipase –> releases fatty acids from chylomicrons and VLDL’s into the tissues.
Lipoproteins can be separated by ultracentrifugation and classified according to their densities.
What are the main functions of chylomicrons?
Describe their composition
Deliver dietary (exogenous) triacylglycerols (TAG) to peripheral tissues.
Highest triacylglycerol, lowest cholesterol

What are the main functions of VLDLs?
Describe their composition
Deliver endogenous triacylglycerols to peripheral tissues.
High triacylglycerols, low cholesterol (less TAG and more cholesterol however than chylomicrons)
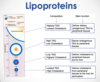
What is the main function of LDLs?
Describe their composition
Deliver cholesterol to peripheral tissues and liver
Low triacylglycerols, highest cholesterol (compared to chylomicrons, LDLs and HDLs)

What is the function of HDLs?
Describe their composition
Deliver cholesterol from peripheral tissues to the liver for elimination.
Lowest triacylglycerol content (compared with chylomicrons, LDLs and VLDLs) and high cholesterol

Describe the exogenous lipid cycle
Dietary lipids absorbed in the GI tract and packaged into chylomicrons which enter the systemic circulation.
Broken down by lipoprotein lipase in the systemic circulation to remove lipid content.
Remnants of chylomicrons reach the liver via the systemic circulation.
Liver breaks down remnants of chylomicrons into cholesterol which is re-introduced to the GI tract via the biliary system.

Describe the endogenous lipid cycle
Fats are endogenously synthesised in the liver —> Lipids are then packaged into VLDL’s and released.
VLDLs released from liver into systemic circulation and broken down by lipoprotein lipase (surface enzyme on the VLDL) into IDLs→LDLs.
LDLs are transported back to the liver and also to extrahepatic tissues, where the majority of the triacylglycerols and triglycerides removed. (Used in metabolism). Removal of triacylglycerols means left with HDL.
HDLs then transport cholesterol back to the liver.

How is cholesterol synthesised?
Cholesterol if synthesised de novo from acetyl-CoA in the liver (80%), intestine (10%) and skin (5%).
Complex regualtory mechanisms ensure cholesterol is only synthesised when needed.
What is the role of cholesterol?
Essential structural component of all cell membranes.
Precursor of steroid hormones (oestrogen, aldosterone, corticosterone, cortisol), bile acids and Vitamin D.
Obtained in the diet and synthesised in the body, most tissues produce cholesterol but the main site of synthesis is the liver.

Describe the composition of most cholesterol
Esterified form, with a fatty acid attached at carbon 3
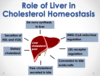
Describe the role of the liver in cholesterol homeostasis
De novo synthesis of cholesterol
HMG-CoA reductase regulation
LDL-receptor regulation
Conversion to bile acids/salts
Secretion of free cholesterol in bile
Secretion of HDLs and VLDLs
Explain “good” vs “bad” cholesterol
“Good” cholesterol –> High density lipoprotein (HDL) –> thought of as good cholesterol as it involves reverse cholesterol transport –> collects cholesterol from peripheral tissues and delivers it to the liver.
“Bad” cholesterol –> Low density lipoprotein (LDL) –> often thought of as bad cholesterol as it is involved in transporting cholesterol from the liver to the extrahepatic tissues where it can become deposited in blood vessel walls –> oxidised + attract inflammatory cells –> atherosclerosis.
Describe the process of cholesterol synthesis in hepatocytes
Acetyl-CoA → Acetoactyl-CoA → HMG-CoA
HMG-CoA broken down by HMG-CoA reductase into Mevalonate (irreversible, the rate-limiting step (slowest))
Mevalonate is transported into the hepatocyte to be converted into cholesterol:
- Mevalonate → C5 → C10 → C15 → C30 → Cholesterol

How do Statins work to reduce cholesterol?
Competitively inhibit HMG-CoA reductase enzyme, therefore slowing down the synthesis of endogenous cholesterol.
A compensatory up-regulation of LDL receptors occurs in an attempt to capture more circulating LDL particles, resulting in decreased plasma LDL
Also lower hepatic VLDL production and increased HDL is sometimes observed

What other beneficial cardiovascular effects do statins have?
What are the side effects and contraindications?
Other beneficial cardiovascular outcomes e.g. lowering plasma fibrinogen and enhancing fibrinolysis and anti-inflammatory effects
Adverse effects:
- GI (e.g. vomiting and diarrhoea)
- CNS (dizziness and blurred vision)
- Muscle (myositis, myalgia, myopathy)
Contraindications:
- Active liver disease
- Pregnancy
- Breast feeding


