Lumbar Spine Flashcards
(61 cards)
upper motor neuron signs
inc muscle tone (spasticity), weakness, hyperreflexia
what is a sign of hyperreflexia
Babinskis sign - big toe is extended rather than flexed upon appropriate stimulation

lower motor neuron signs
muscle weakness, wasting (atrophy), absence of reflex
how do spinal nerves arise
- begin as anterior (motor) and posterior (sensory) nerve root, arise from spinal cord and unite at intervertebral foramina, forming a single mixed spinal nerve
- The spinal nerve then leaves the vertebral canal via the intervertebral foramina and divides into two:
- The posterior rami supply the nerve fibres to the synovial joints of the vertebral column and the deep muscles of the back, and the anterior rami supply nerve fibres to much of the remaining body (posterior = dorsal).

where does the mixed spinal nerve splt into posterior and anterior rami
intervertebral foramina


at what level does the spinal cord end
- L1/2 - tapers off forming the conus medullaris
- the spinal nerves that arise from here are called the cauda equina
- therefore, there is no spinal cord in the lumbosacral spine - problems here tend to arise as nerve root problems not spinal cord injury

which nerve root is commonly affected in disc prolapse
- traversing nerve root
- in far lateral disc prolapse the exiting nerve root can be affected
how are nerve roots named in the cervical and lumbar spine
In the cervical spine, the nerve root is named according to the lower spinal segment that the nerve root runs between, e.g. nerve at C5-6 level is called C6 nerve root.
In the lumbar spine, the nerve roots are named according to the upper segment that the nerve runs between.
what does nerve root compression cause
radiculopathy (pinched nerve) that results in pain down the dermatome of that nerve, and weakness ina ny muscle supplied (myotome) with reduced or absent reflexes
what is nerve root compression called in the lower leg
sciatica (L4-S3)
sciatica - L3/4 prolapse

(L4 entrapment)
pain down to medial ankle, loss of quadriceps, reduced knee jerk
sciatica - L4/5 prolapse
pain down dorsum of foot, reduced power extensor hallicus longus and tibialis anterior

sciatica - L5/S1 prolapse
pain to sole of foot, reduced pwoer plantarflexion, reduced ankle jerks

what can a very lateral disc prolapse cause
impingement of the exiting nerve root

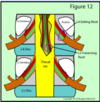
A – laterally placed prolapse affects exiting nerve root (e.g. exiting L4).
B – central prolapse affects traversing nerve root (e.g. traversing L5).
C – central prolapse leads to cauda equina.
D – formation of osteophytes in the lateral canal will also lead to root compression.
treatment of disc prolapse
analgesia, maintaing mobility and physio are first line
drugs for neuropathic pain (gabapentin) in severe cases
very occasionally surgery (discectomy)
within what time period should disc prolapse resolve
3 months
after this surgery (discectomy) may be considered
chance fractures
- seatbelt fractures
- sudden flexion of the vertebral body disrupts the posterior elements
- very unstable and associated with intra-abdominal injuries


chance fracture
where is lumbar puncture and spinal anaesthesia performed
highest point of iliac crest - L4
myelopathy
- describes any neurologic deficit related to the spinal cord
- causes upper motor neuron signs eg Babinski sign
babinski sign
the big toe is extended rather than flexed on appropriate stimulation
upper motor neuron symptom

spondylosis
broad term meaning degeneration of the spinal column
intervertebral discs lose water content with ageing leading to overloading of the facet joints
most commonly occurs L45 and L5/S1














