Membranes, Nerve, Muscle and Neurophysiology Flashcards
(57 cards)
What is the nernst equation with regards to its importance in membrane physiology?
The nersnst equation describes the electrical potential that opposes the diffusion of a molecule across a membrane. Ions will want to move in the directoin that brings them closer to this potential (equilibrium).

For each of the following molecules, indicate which is more prevalent inside vs. outside the cell:
- Sodium
- Potassium
- Chloride
- Magnesium
- Bicarbonate
- Phosphate
- Amino acids and proteins
- Glucose
- Lipids (e.g. cholesterol, phospholipids)
- Outside
- Inside
- Outside
- Inside
- Outside
- Inside
- Inside
- Outside
- Inside
How does urea move through the cell membrane?
Urea is highly permeable through cell membranes.
What are the selecitivty filters of the following channels?
- Na
- K
- Negatively charged amino acids - attract Na ions
- Carbonyl oxygen which removes water from hydrated potassium ions to allow them to pass through the channel
How will the rates of diffusion differ for facilitated vs. simple diffusion?
How does this differ when considering physiologic membranes?
Facilitated will reach a maximum, likely due to the rate at which the proteins in the channels can change shape.
Simple diffusion will always increase rate of diffusion in a linear fasion.
Membrane permeability will affect the movement of the substance in question when in a physiologic medium.

Name the three factors that affect rate of diffusion of charged molecules?
- Concentration
- Nernst potential
- Pressure
What is the membrane potential of most membranes?
-70mV
What channels are present in the cell that contribute to the resting membrane potential?
Na/K-ATPase
K leak channels - these allow free movement of potassium. Since the Na/K pump moves positive ions out of the cell in greater quantity to those coming in, the potassium will reach and equilibrium potential under resting conditions.
This is why changing ECF potassium concentrations can change the resting membrane potential. The resting potential becomes more negative with low ECF potassium as there is a lower concentration gradient for potassium to move into the cell.

Explain the events that occur in the membrane of cells during action potential with reference to sodium and potassium channels.
- ‘Fast’ sodium channels open which are inactive at -70mV but are activated and open following stimulus.
- These become inactive again (through a different mechanism) when the membrane potential becomes positive again.
- They return to their resting state only when the membrane has reached resting potential again.
- Potassium channels will also be activated when there is an action potential but they are much slower to open and therefore the net movement of sodium is much quicker than potassium during depolarisation.
How does ECF calcium concentration affect membrane exitability?
It is thought that Ca binds to the exterior of sodium channels and affects the voltage required to open them. This is how the calcium affects threshold potentials.
e.g. Hence why low calcium causes hyperexitability as it means depolarisation is more likely to occur.
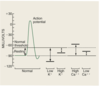
What is the value of the normal threshold potential?
15-30mV
Why are cardiac action potentials so much longer than nerve action potentials?
L-type calcium channels are present in the physiology of cardiac muscle contraction. These act in a similar way to sodium channels but are much slowe to open and close.
Potassium channels in cardiac muscle also seem to open and close slower.
How might action potentials be elicited by a stimulus?
Either with a large stimulus or a more frequent stimuli.
What is the molecular mechanims of the refractory period?
This is the period in which the sodium (or calcium) channels inactivation gate is closed. This will only re-open once the membrane reaches its resting potential again.
Explain the following terms in relation to skeletal muscle anatomy:
I bands
A bands
Z disk
Sarcomere
Titin
I = the layers of actin only
A = where actin and myosin overlap
Z = protein filament that attaches to actin
sarcomere = the space between z-discs
Titin = the springy filament that connexts the z-disk to myosin

Where in the actomyosin complex is ATPase activity located?
In the myosin head.
What are the structural elements of the actin filament?
F-actin = the main structural element tha contains ADP molecules at binding sites
tropomyosin - this covers the binding sites
What are the components of the troponin complex?
I - binds to actin
t = binds to tropomyosin
c = afinity for calcium
How many calcium ions can be bound by each troponin C molecule?
4
Explain the cross-bridge theory of muscle contraction
- Calcium binds to troponin C exposing the F-actin binding sites
- ATP –> ADP + P by the ATPase on the myosin molecule which results in the head tilting towards the binding site.
- Upon binding the power stroke occurs.
- ADP + P leave the myosin
- A new ATP binds to the myosin which allows it to detach from the actin filament.
What is the relationship of actin overlap to tension that can be created through a muscle?
If there is too much overlap then less tension is produced.
Explain the following terms:
- Multiple fibre summation
- Frequency summation
Summation is the addition of contractions to increase intensity of contraction
- Increased umber of motor units that fire at the same time
- Increasing the frequency at which motor units fire
What is the mechanism by which calcium entry into a cell results in the movement and exocytosis of vesicles?
Calcium activates Ca2+-calmodulin–dependent protein kinase, which, in turn, phosphorylates synapsin proteins that anchor the acetylcholine vesicles to the cytoskeleton of the presynaptic terminal. This process frees the acetylcholine vesicles from the cytoskeleton and allows them to move to the active zone of the presynaptic neural membrane adjacent to the dense bars
How many Ach molecules are required to activate sodium channels on the motor end plate?
2





