microcytic anaemia Flashcards
(31 cards)
definition of microcytic anaemia
Anaemia associated with low MCV (<80 fl).
aetiology of microcytic anaemia
iron deficiency commonest cause
anaemia of chronic disease - often normocytic, can be monocytic
thalassaemia
sideroblastic anaemia
lead poisoning (eg in scrap metal or smeltering workers) - interferes with globin and haem synthesis
aetiology of IDA
blood loss eg GIT, urogenital tract, hookworm infection, menorrhagia
reduced absorption - small bowel disease, post-gastrectomy, coelic (refractory IDA)
increased demand - pregnancy, growth
reduced intake - vegans, poor diet or poverty in children
sideroblastic anaemia
abnormality of haem synth
can be inherited (x-linked)
secondary to alcohol, drugs (eg isoniazid, chloramphenicol), lead, myelodysplasia/myeloproliferation
chemo
irradiation
alcohol
NOT IRON DEFICIENT
epidemiology of microcytic anaemia
Iron-deficiency anaemia is the commonest form of anaemia worldwide.
sx of microcytic anaemia
tiredness
lethargy
malaise
dyspnoea
pallor
exacerbation of pre-existing angina or intermittent claudication
FH of causitive disease
lead poisening sx
anorexia
nausea
vomiting
abdominal pain
constipation
peripheral nerve lesions
signs of microcytic anaemia
signs of anaemia
- pallor of skin and mucous membranes
- brittle nails and hair
- if long standing and severe - koilonychia
glossitis - atrophy of tongue papillae
cheilitis - angular stomatitis
signs of thalassaemia
signs of lead poisoning
signs of lead poisoning
blue gumline
peripheral nerve lesions - wrist/foot drop
encephalopathy
convulsions
reduced consciousness
Ix for microcytic anaemia
blood
blood film
Hb electrophoresis
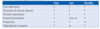
blood results if microcytic anaemia
FBV - low Hb, low MCV, reticulocytes
serum iron - low in ID
iron binding capacity - increased in ID
serum ferritin - low in ID
serum led - if poisoning suspected
in thalassaemia and sideroblastic anaemia - hogh serum iron and ferritin and low total iron binding capacity
blood film in IDA
microcytic, hypochromic (central pallor >1/3 cell size),
anisocytosis (variable cell size)
poikilocytosis (variable cell shape)
blood film in sideroblastic anaemia
dimorphic blood film with a population of hypochromic microcytic cells
blood film for lead poisoning
basophilic stippling - coarse dots represent condensed RNA in cytoplasm
Hb electrophoresis for microcytic anaemia
for Hb variants for thalassaemias
sideroblastic anaemia
- ring sideroblasts in bone marrow, iron deposited in perinuclear mitochondria of erythroblasts, stain blue-green with Perls’ stain
Ix if iron-deficiency anaemia in>40 years and post-menopausal women
upper GI endoscopy
colonoscopy
investigations for haematuria
all should be considered if no obvious cause of blood loss
Mx for IDA
oral iron supplements eg 200mg ferrous sulphate tablets containing 65mg of elemental iron, 2 or 3x daily taken with food
SE - nausea, abdo discomfort, diarrhoea/constipation, black stools
If oral iron intolerance or malabsorption or functional iron deficiency in chronic renal failure where inadequate mobilisation of iron stores in response to erythropoetin therapy - consider parenteral iron supplements (beware risk of anaphylaxis).
monitor Hb and MCV, aiming for Hb rise of 1g/dL/week. Modest reticulocytosis
continue for at least 3mo
Mx of sideroblastic anaemia
treat the cause - stop causative drug
pyridoxine can be used in inherited forms
if no response - blood transfusion and iron chelation
Mx of lead poisoning
remove source
dimercaprol
D-penicillamine
Ca2+ EDTA
complications of microcytic anaemia
high output cardiac failure
complications of the cause
prognosis of microcytic anaemai
depends on cause
signs of IDA
koilonychia
atrophic glossitis
angular cheilosis
post-cricoid webs (Plummer-Vinson syndrome)
Ix results for IDA
blood film:
- microcytic
- hypochromic anaemia
- anisocytosis
- poikilocytosis
blood
- low MCV, MCH< MCHC
- low ferritin
- low iron
- high TIBC (transferrin)
check coelic serology - if -ve refer men adn women not menstruating to gastroscopy and colonscopy
stool microscopy for ova if relevant travel history

ferritin
acute phase protein
increases with inflammation eg infection and malignancy