Mod IV: Regional Anesthesia Part 5 Flashcards
(70 cards)
Regional Anesthesia - Locating Nerves
How to find what your looking for?
Apply that Anatomy
Knowledge of nerve path, surrounding structures, and surface landmarks is of paramount importance
Regional Anesthesia - Locating Nerves
Techniques used to localize nerves
Landmarks - Paresthesia - Nerve Stimulator
Ultrasound - Fluoroscopy
CT guided
Regional Anesthesia - Locating Nerves
Nerve localization technique that provides both still and live x-ray views:
Fluoroscopy
Used primarily in pain blocks
Expensive
Regional Anesthesia - Locating Nerves
Nerve localization technique that provides still and live Ct images:
Ct guided
Used rarely in pain blocks
Extremely expensive!!!
Regional Anesthesia - Locating Nerves
Techniques for locating nerves that use surface landmarks and knowledge of anatomical relationships:
Landmark Techniques

Regional Anesthesia - Locating Nerves
Using Landmarks alone can help anesthetized which structures?
Ankle
Digits
Cervical plexus

Regional Anesthesia - Locating Nerves
Landmark Techniques can be combined with:
Paresthesia
Nerve Stimulator
Ultrasound
Regional Anesthesia - Locating Nerves
The feeling of tingling, tickling, burning, prickling, or buzzing felt is also known as:
Paresthesia
Regional Anesthesia - Locating Nerves
What’s the goal of Paresthesia technique?
To place the needle in direct contact with the desired nerve to produce a Paresthesia
This tells the practitioner they are very close or in the target nerve, then withdraw slightly until paresthesia stops and inject LA
NEVER inject LA if pt has sharp PAIN or PARESTHESIA!!!
The elicited paresthesia should follow the target nerves distribution
Old technique still used by some practitioners
Regional Anesthesia - Locating Nerves
What are disadvantages of the Paresthesia technique?
Risk of neural injury
Higher block failure rates when compared to newer techniques
Regional Anesthesia - Locating Nerves
Nerve localization technique that uses electricity to produce a response of a target nerve:
Nerve Stimulator Technique
Used in combination with anatomical and surface landmark knowledge
Motor –Target nerve muscles twitch
Sensory – paresthesia over target nerve distribution

Regional Anesthesia - Locating Nerves
Membrane potentials - What’s Resting MP?
– 90 mV

Regional Anesthesia - Locating Nerves - Membrane potentials
What’s Threshold Level? what happens when it’s reached by a stimulus?
– 55mV
Depolarization occurs
Propagation of Action potential
Regional Anesthesia - Locating Nerves
How does Nerve Stimulator work?
Negative Polarity Impulse
Neutralizes positive current outside nerve dropping MP
Black lead attached to needle
Red positive lead is attached to skin

Regional Anesthesia - Locating Nerves
Which nerves have Lowest Threshold of Ext Stim to generate AP? why?
Motor nerves
B/c Highly myelinated nerves

Regional Anesthesia - Locating Nerves
Which nerves have Higher Threshold for External Stim to generate AP? why?
Sensory nerves
B/c Unmyelinated nerves – slower

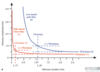
Regional Anesthesia - Locating Nerve - Generating a Action Potential
Which characteristics of a stimulus determine generation of an Action Potential?
Stimulus Strength and Duration

Regional Anesthesia - Locating Nerves
Generating a Action Potential - Strength of electrical stimulus is also known as:
Current Amplitude

Regional Anesthesia - Locating Nerves
The amount of time a stimulus must be applied to generate an Action Potential is known as:
Current Duration
Regional Anesthesia - Locating Nerves
Generating a Action Potential - Impulses of which duration are better discriminator of distance?
Short duration impulses
Regional Anesthesia - Locating Nerves
Motor impulse duration:
0.1 ms

Regional Anesthesia - Locating Nerves
Sensory impulse duration:
0.3 ms
Longer duration needed to reach threshold level

Regional Anesthesia - Locating Nerves
Nerve stimulator - Frequency:
1-2 Hz
Regional Anesthesia - Locating Nerves
Nerve stimulator - Duration:
- 1ms Motor
- 3 ms Sensory




























