What does sessile mean?
Flat - though can have villous architecture
What does pedunculated mean?
On a stalk, somewhat resembling a mushroom.
What are three types of non-neoplastic colorectal polyps we covered?
•Hamartomatous polyps
- Inflammatory Polyps
- Hyperplastic Polyps
What are three neoplastic colorectal polyps we discussed?
- Sessile serrated Adenoma
- Adenoma
- Polyposis Syndromes when numerous polyps are present
Hamartomatous Polyps have a haphazard arrangement of normal stromal and epithelial elements. What do they occur mainly as a result of?
Why is it important to recognize these polyps?
- Occur mainly as a component of a polyposis syndrome but can occur as a sporadic hamartomatous polyp
- It is important to recognize these polyps because of associated intestinal and extraintestinal malignancies.
What are two polyp syndromes that give rise to hamartomatous polyps?
–Peutz-Jegher syndrome
–Juvenile polyposis
Is Peutz-Jegher syndrome heritable?
Yes - Autosomal Dominant
What are the physical manifestations of Peutz-Jegher syndrome?
Multiple GI hamartomatous polyps and mucocutaneous hyperpigmentation.
Where do the polyps of Peutz-Jegher syndrome most often appear?
Small intestine
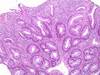
What has this kid got going on?

Peutz Jegher Syndrome
What was the cause of this polyp?
How do you know?

Peutz Jegher Syndrome
Small intestine Peutz Jegher polyps have a smooth muscle core with arborizing branches. Most polyps have a connective tissue core, so this is pretty distinct.
What do you get the pleasure of telling this patient about his disease?

Peutz-Jegher syndrome has a marked increased risk of malignancies.
Ok, so we established that Peutz-Jegher syndrome has a marked increased risk of malignancies. Which ones?
What is the total lifetime % risk?
- Colon
- Pancreas
- Breast
- Lung
- Urinary
- Gynecologic
40% lifetime risk
What condition does this person have?
What is being stained in the image on the right?

Peutz-Jegher syndrome
Muscle actin stain - reveals arborizing smooth muscle
The majority of juvenile (retention) polyps occur in children younger than 5 years of age. Describe the malignancy potential of this condition.
If solitary (which is 70% of the time): virtually no malignant potential
Can hovever be associated with dysplasia, and 30 - 50% develop colonic adenocarcinoma by 45.
What is the inheritance pattern of juvenile (retention) polyps?
Autosomal Dominant
This was removed from the colon of a 5 year old patient, it was the only polyp found. Is it malignant?

Almost certainely not - Juvenile Polyposis
This lesion was removed from the colon area of our patient who has a 3 year history of ulcerative colitis. What is it?
Inflammatory polyp
Inflammatory polyps are found in the regenerative and healing phases of inflammation. What disease states give rise to this?
Severe colitis
chronic inflammatory bowel disease
ameobic colitis
ischemic colitis
bacterial dysentery
Solitary rectal ulcer syndrome
This was obtained from a patient’s left colon/rectum in their 60/70s, This is the most common type of colon polyp.
What is it?
Is it malignant?

Hyperplastic polyp
Benign
(left colon/rectum import for distinguishing from sessile serrated adenoma)
What is the most common type of colonic polyp?
Whe is it typically discovered?
Hyperplastic polyp
6th to 7th decade of life
You find multiple polyps in your patients right colon, some of which are greater than 5mm. What are there?
What is/are the mutations commly in?
How is this patients outlook?
Sessile serrated adenoma (the right colon bit is important)
High rate of BRAF mutations and DNA methylation
Patients with multiple serrated polyps are at an increased risk of colonic adenocarcinoma.
Sessile serrated adenoma are most commonly found in the right colon. What does it typically resemble histologically?
What is one way to distinguish?
Resemble hyperplastic polyp
Hyperplastic polyp - Left colon/rectum
Sessile Serrated adenoma - Right colon
Conventional adenomas are common lesions that are almost always asymptomatic, the clinical importance of these lesions is related to?
Their well established premalignant nature
50% of the the population >50 yo in Western countries such as the United States have adenomas. Size of the lesion is a strong predictor of progression to malignancy. How big do they have to be to have a substantial increase in the risk of malignancy?
Greater than 2 cm
What is the appropriate treatment of colorectal adenomas?
What is the optimal screening tool for this?
Complete removal.
Colonoscopy is the gold standard
At what age do most people need to start colorectal screening?
50 y/o
What is shown here?

Pedunculated tubular adenoma
What does the attached histology depict?

Tubular adenoma - note the sircular formations
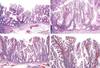
Identify the adenomae shown in images A and B.

A. Tubular: The polyps have a dome-shaped surface. The largest polyp in the center also shows subtle lobulations.
B. Villous: The polyp grows as a flat plaque with slightly raised edges. (sessile)
What is this?
Villous adenoma
This image illustrates characteristic findings in a villous adenoma. What are they?
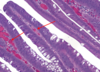
Villous adenomas are characterized by slender papillae containing a fibrovascular (arrows) core and lined by adenomatous epithelium
What are the risks of cancer in a polyp that is the following sizes?
1 - 2 cm
> 2cm
> 4cm
–Between 1-2 cm 5% risk of cancer
–> 2 cm 10-20% risk of cancer
–> 4 cm 40% risk of cancer
Which adenoma is more likely malignant, villous or tubular?
Villous
The severity of epithelial dysplasia increases the odds of a polyp being malignant. Does it increase the risk of carcinoma elsewhere in the colon?
No
What is shown in the circle sign?
How do you treat it?

Cancer in an adenomatous polyp.
Treat by removing the polyp since it is not in the stalk or near the base.
If cancer appears in a polyp close to the margin, how do you treat then?
Either…
Post polyp removal, burn the crap out of the residual mucosa
Or
Remove 10 cm of bowel around the lesion
What is the inheritance pattern of familial adenomatous polyposis?
Autosomal dominant
What is FAP characterized by?
•presence of hundreds to thousands of adenomas in the colorectal mucosa by 20 to 30 years
FAP is the result of an inheriteddefect in what?
One allele of the APC tumor suppressor gene
What does this look like?
What was the inciting event?

Familial Adenomatous Polyposis
APC mutation kicked it off
What have we here?

FAP!
What is Lynch syndrome?
Lynch Syndrome
Hereditary Nonpolyposis Colorectal Cancer (HNPCC)
Roughly 3% of CRC can be linked to Lynch syndrome, what is is the life time risk?
~80%
What is the general onset of lynch syndrome?
Mean age 44 years
Lynch syndrome occurs secondary to what mutations?
Germline mutations in DNA mismatch repair genes
Lynch syndrome is also associated with other cancers, including what 4 things he specifically listed?
- Endometrium
- Ovaries
- Pancreas
- Stomach
Which is due to microsatellite instability and which d/t chromasome instability?
Lynch Syndrome - Microsatellite instability
FAP - Chromosomal Instability
What is the classic adenoma-carcinoma sequence?
Normal Colon: “First hit” - Germline or somatic mutations of - APC at 5q21
Mucosa at risk: “Second hit” - Methylation abnormalities with inactivation of normal alleles
Adenomas: Proto-oncogene mutations - KRAS at 12p12
Adenomas: Homozygous loss of additional suppressors with over expression of COX-2 (TP53)
Carcinoma: Additional mutations gross chromosomal alterations.

Colorectal adenocarcinoma hits males more than females. How does it begin?
When does it usually present?
- Begin as intramucosal epithelial lesions, usually arising in adenomatous polyps or glands
- Average age at diagnosis in seventh decade of life (5th decade for HNPCC)
What is the most effective treatment for early stage colorectal adenocarcinoma?
What is the 5 year survival rate?
Does this tend to metastasize?
- Surgical resection most effective treatment for early stage (T1 and T2)
- 5-year survival rate 55% to 60%
- Metastases are common
What percent of sporadic colon adenocarcinoma does the “classic” adenoma-carcinoma sequence account for?
80%
If colorectal cancer starts out as a flat cancer without a polyp, what was likely mutated first?
P53
What is this finding?
What is it d/t?
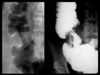
Apple core sign
Colon adenocarcinoma
How likely is this colorectal carcinoma to metastasize?
Why?

Very likely, since it has penetrated the serosa
These are images you took during a procedure to remove polyps from a persons colon. What was the last thing you did before you pulled the scope out and went home?

Injected india ink to stain the site, in case you have to go back again you’ll be able to find the area easily.
What do each of the arrows indicate in this tubulovillous adenoma?

Left: Adenoma
Right: Carcinoma
What type of adenocarcinoma is described here?
The neoplasm forms uniform gland structures, and the nuclei are localized to the basal half of the neoplastic cells.
Well-differentiated carcinoma
What level of differentiation?
The neoplasm is composed of complex glandular structures, with loss of polarity of the nuclei. Most colorectal carcinomas are moderately differentiated.
Moderately differentiated carcinoma
What level of differentiation?
The carcinoma shows minimal to no gland formation.
Poorly differentiated carcinoma
Colorectal carcinoma grow slowly and may be present for as long as 5 years before symptoms appear. Asymptomatic persons often have occult blood loss from their tumors. They may have constitutional symptoms, including fatigue, shortness of breath, and angina.
What are these symptoms d/t?
Microcytic hypochromic anemia
Colorectal carcinoma is often misdiagnosed in patients, as…
•diverticular disease (abdominal pain, bleeding, change in stool caliber), IBS (abdominal pain, change in bowel habits), or hemorrhoids (rectal bleeding)
Thus it is important to?
Biopsy any wierdness you find
Describe the findings you see in this image taken from a patients colon.

Infiltration of malignant glands indicates invasive colon carcinoma. This is a “well differentiated” tumor, according to Brozna and the notes section.
What is shown here?

LefT: Lymph node metastasis with lymphatic channel adenocarcinoma spread.
Right: Artery Intraluminal adenocarcinoma
What is shown here?
Adenocarcinoma to the lymph node
Where does colorectal cancer tend to metastasize to?
The liver
Although uncommon, small intestine tumors do occur. What are three examples of benign small intestine tumors?
–Hyperplastic polyp
–Hamartoma
– Adenoma
As mentioned before, small intestine tumors are uncommon in comparison with those occurring elsewhere in the GI tract. What are some examples of malignant tumors of the small intestine?
5
- Adenocarcinoma
- Carcinoid
- Lymphoma
- Gastrointestinal Stromal Tumors (benign and malignant)
- Metastases (50% of small intestine tumors)
How are most benign small intestine tumors found?
Incidentally
Where do most small intestine adenocarcinoma/adenoma occur?
ampulla of vater in the duodenum
What is the most common small intestine malignancy?
Carcinoid tumors (neuroendocrine)
Via what cell line are most small intestine lymphomas derived from?
B-cell
Does celiac disease increase the risk of small intestine adenocarcinoma?
Yes, 80 fold
What percent of intestinal adenomas arise in the small intestine?
< 0.05%
Which is more common in the small intestine, primary neoplasms or metastatic tumors?
Metastatic tumors
What cells do neuroendocrine tumors arise from?
•enterochromaffin cells (Kulchitsky Cells)
What are the most common sites of carcinoid tumors?
Ileum
Appendix
What often leads to discovery of carcinoid tumors?
•Often are identified by symptoms caused by the hormones they secrete
What is the most important factor prognostically in carcinoid tumors?
Location
What locations are positive prognostic indicators for carcinoid tumors?
Esophagus
Stomach
(rarely metastasize, and generally resectable)
What locations serve as bad prognostic indicators for carcinoid tumors?
Jejunum
Ileum
(often multiple and tend to be aggressive)
Classical carcinoid syndrome appears in 10% of patients and consists of what clinical symptoms?
- Severe episodic skin flushing
- Diarrhea, abdominal cramping
- Asthma, bronchoconstriction
- Rapid heart rate and tricuspid valve insufficiency
Carcinoid syndrome requires tumors put hormones into non-portal venous circulation and are therefore strongly associated with metastatic disease.
What are five examples of hormones produced by these tumors?
- Serotonin,
- 5-hydroxytryptophan,
- kallikrein,
- histamine,
- prostaglandins
What is depicted here?

Carcinoid syndrome
How would you describe this carcinoid tumor of the ileum?

Invasive - extends through the muscularis propria to involve the serosal connective tissues
What are somet things to watchout for on histology and as buzzwords in question stems for neuroendocrine tumors in general?
Salt and pepper chromatin
Zell Ballen
What does one call the membrane bound neurosecretory granules with an electron dense core and a halo produced in carcinoid tumors?
Dense core granules
What is a cloacogenic carcinoma?
Old term for poorly differentiated squamous cell carcinoma (basaloid growth pattern)
What are the main malignant tumors of the anal canal?
Adenocarcinoma
Squamous cell carcinoma
Melanoma
Where in the anal canal do adenocarinomae typically present?
Upper third
Where do squamous cell carcinomae typically present in the anal canal?
Lower third
What are many instances of squamous cell carcinoma associated with?
HPV
Describe the anal tumor shown attached.
Basaloid (cloacogenic) squamous cell anal carcinoma
The vermiform appendix arises from the cecum and has no known specific function (except possibly serving as a micriobiome reservoir from which normal flora can grow to reestablish themselves after infections are cleared), is 6-7 cm long in the adult, and is rich in what?
Lymphoid
Acute appendicitis is largely a disease of the industrialized world, and mostly of adolescents and young adults. Males tend to be affected slightly more often, and the over all lifetime risk is around 7%.
What are the classical clinical findings?
- initial peri-umbilical pain, localizing to right lower quadrant (McBurney sign)
- nausea and/or vomiting
- abdominal tenderness, rebound
- mild fever
- leucocytosis (15,000 – 20,000/cu.mm)
The false positive rate for acute appendicitis was once 20 - 25%. What is it now, and why?
•Routine use of preoperative computed tomography (CT) has decreased false positive rate to ~3%
What is a common cause of acute appendicitis?
Fecalith
What is this?
What can it cause?

Mucinous cystadenoma
pseudomyxoma peritonei - gelatinous ascites
What is the most common tumor of the appendix?
Carcinoid most common
Apart from carcinoid tumors, what other tumors affect the appendix?
- Typical bowel Adenomas and Adenocarcinomas, uncommon
- Mucinous cystadenoma (mucocele)
What are some examples of things that cause peritonitis? 5
- Leakage of bile or pancreatic enzymes (sterile/suppurative/hemorrhagic)
- Foreign material (talc) especially post-op (granulomatous)
- Endometriosis (sterile)
- Ruptured dermoid cysts (granulomatous)
- Perforation of abdominal viscera (Suppurative)
What is the most common primary tumor of the peritoneal cavity?
•Mesothelioma is most common primary malignancy, and almost always associated with asbestos exposure
What are some cancers that hit the peritoneal cavity by direct spread or metastatic seeding?
- Ovary
- Colon
- Pancreas
- Appendix
- Leiomyosarcoma
- Liposarcoma

