Pathology-Final MSK Review Flashcards
(31 cards)
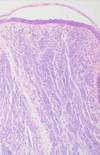
What characteristics of this slide tip you off that this patient has a contact dermatitis

Spongiosis, intraepidermal blistering, and mononuclear infiltrate.
What characteristic of keratinocytes tip you off when looking at a squamous cell carcinoma?
There will be desmosomes between the malignant cells.
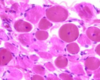
What is your diagnosis? What is causing this patient’s condition?

This is pemphigus vulgaris. Note the “tombstone” basilar cells that remain. It is an autoimmune reaction to desmoglein. This causes round acantholytic cells.

What is the whole spectrum of this disease?

Skin (erythema multiforme from herpes infection), mucosal involvement (Stevens-Johnson from drug reaction), whole body involvement (toxic epidermal necrolysis).
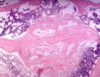
What is your diagnosis? What leads you to this decision?

This is psoriasis. Notice hyperkeratosis, parakeratosis, Munro microabscesses, acanthosis and rete ridges.
What is this “wisdom disease”? How does it look clinically?

This is seborrheic keratosis. Note the flat top, broad and flat epidermis with little horn cysts.

A patient presents to your clinic with this lesion. It dimples when you squeeze it. How deep do you need to go when excising this tumor?

This is dermatofibroma. You will have an increase in basal pigmentation and fibroblastic proliferation deep in the dermis traps collagen bundles…thus you need to cut it deep.

What features about this lesion guide your diagnosis? How might this lesion look under a microscope?

A well circumscribed, ulcerating lesion with telangectasia directs your thoughts toward basal cell carcinoma. Notice no change in granular layer with palisading, small-nucleated cells that collect in the middle of the dermis.

What is the most common carcinoma of the skin? What is the prognosis?
Basal cell carcinoma. They often occur in sun-exposed areas and are benign.
A patient presents to your clinic with this lesion on his hand. How does this disease progress?

It starts as actinic keratosis to squamous cell carcinoma in situ (fully unmaturated cells localized to epidermis) to squamous cell carcinoma (breaks through basement membrane)

What are the different benign nevi? How would you stain for these melanocytes?
Junctional, compound and dermal. You stain with S100 because it is specific for neural cells…which melanocytes differentiate into.
What determines if these nevi are becoming a malignant melanoma?

Pagitoid spread of melanocytes, high nuclei to cytoplasm ratio, melanocyte infiltrate into dermis without differentiation, and Breslow level above 1mm as seen below.

Why is it important to get his entire lesion?

It is an epidermal inclusion cyst, full of inflammatory cells.
How would you stain this skin biopsy?

GMS (silver stain) or PAS (periodic acid shift) will show you fungi living in the intradermal layer of tinea corpus.

What is your diagnosis?

Vulgaris. Notice hyperkeratotic and aconthotic layers of epidermis and dermis respectfully.
What causes pseudo hypertrophy in this patient?
Note increase in connective tissue between muscle fibers in muscular dystrophy. This patient will have an absence of dystrophin.

What cells are causing muscle destruction in these images?

Top = CD4+. Bottom CD8+
Whats going on here?

Dennervation atrophy
What immunohistochemical stain is used here?

Desmin. This is specific for tumor cells in rhabdomyosarcoma. This is necessary because it is in the family of small round blue tumors as seen below.

This woman has osteoporosis. What is going on in this slide of her vertebra?
This is pro callus (clot) formation after a micro fracture.
What do you expect to see histologically in this section?

Rough surface due to weakening and loss of cartilage (fibrillation). The cartilage can also break off into the joint to form joint mice. You may also see subchondral cysts.

What is being made by the tumor cells in this lesion? What genes put you at higher risk for this condition?

This is osteosarcoma. Osteoid is being laid down by the osteoblasts in trabecullae. RB and p53 put you at higher risk.

How would this lesion look microscopically? Where do these lesions normally occur?

This is a chondrosarcoma. Note hyper cellular and less cellular areas organized into lobules. Also note multiple chondrocytes in lacunae. The often occur in the axial skeleton.

How does this lesion look radiographically? Histologically?

This is Ewing sarcoma. It will have onion skin layering because it is a slow growing tumor. Histologically you will see Homer-Wright rosettes (more common in PNET) and neural cells.








