What is the alimentary canal?
A series of hollow organs running from mouth to anus that are separated by sphincters, controlling movement
Describe the structures ‘food’ passes through in the alimentary canal from start to finish
- Mouth & oropharynx
- Oesophagus
- Stomach
- Small Intestine
- Large Intestine
- Rectum & Anus
What are the accessory structures of the alimentary canal?
- salivary glands
- the pancreas
- the liver and gall bladder (hepatobiliary system)
Describe the basic activity of the mouth and oropharynx
- chops and lubricates food
- breaks down by saliva secreted by salivary glands
- starts carbohydrate digestion
- secretes alpha amylase which begins process of digestion of materials such as starch
- propels food to oesophagus
describe the basic activity of the oesophagus
it’s a muscular tube
- propels food by peristalsis to stomach
Describet the basic function of the stomach
- stores & churns food
- only allows progression of semi-digested food
- churning mechanical activity mixes food with enzymes
- continues carbohydrate and initiates protein digestion
- c comes before p in alphabet
- pepsin breaks down proteins
- regulates delivery of chyme to duodenum
Describe the basic function of the small intestine
*duodenum, jejunum and ileum*
- principal site of digestion and absorption of nutrients
- secretions from intestine and pancreas to make aqueous
- ?! i thought in later lecture he said small intestine doesnt secrete ?!
Describe the basic function of the large intestine
*caecum, appendix and colon*
- leftover products which have not been absorbed
- initially in the caecum and then to part of the colon e.g. ‘descending transverse blah blah blah’
- colon
- reabsorbs fluids and electrolytes
- stores faecal matter before delivery to rectum
- condenses and dries out matter; good healthy fairly solid stool delivered to rectum
What are the basic functions of the rectum and anus?
- storage and regulated expulsion of faeces
What are the four main parts of the structure of the digestive tract wall
- Mucosa
- Submucosa
- Muscularis Externa
- Serosa
NB: specialisations occur in specific regions (e.g. additional oblique smooth muscle layer in stomach)

What cells make up the mucosa?
- epithelial cells
- exocrine cells
- endocrine gland cells
- lamina propria
- capillaries
- enteric neurones
- immune cells
- muscularis mucosae
What the cells make up the submucosa?
- connective tissue
- larger blood and lymph vessels
- glands
- nerve network
- submucos plexus
What makes up the muscularis externa?
- circular muscle layer
- nerve network
- myenteric plexus
- longitudinal muscle layer
What is the serosa?
connective tissue
What are the four main activities of the alimentary canal?
1. Motility
- mechanical activity mostly involving smooth muscle (skeletal at mouth, pharynx, upper oesophagus and external anal sphincte
2. Secretion - into the lumen of the digestive tract occurs from itself and accessory structures in response to the presence of food, hormonal and neural signals
- required for:
- digestion
- protection
- lubrication
- mucin absorbs water and then becomes mucous
- Digestion
- chemical breakdown by enzyme hydrolysis of complex foodstuffs to smaller, absorbable, units
- NB: physical digestion in the mouth, stomach and small intestine contributes
- Absorption
- Transfer of the absorbale products of digestion (with water, electrolytes and vitamins) from digestive tract to the blood, or lymph
- vast majority of diet is not absorbable but needs broken down first
- in case of carbohydrates only monomers can be directly absorbed
- largely mediated by numerous transport mechanisms
What are the muscles layers most important for gastrointestinal motility?
- circular
- longitudinal
- muscularis mucosae
NB: skeletal muscle is important in the mouth, pharynx, upper oesophagus and external anal sphincter
How does contraction of the
a) circular muscle
b) longtidunal muscle
c) muscularis mucosae
affect the intestine?
a) lumen becomes narrower and longer
b) intestine becomes shorter and fatter
c) change in absorptive and secretory area of mucosa (folding). mixing activity
Describe the structure and layout of smooth muscle cells in the GI tract.
- smooth muscle cells are coupled by gap junctions
- allows spread of electrical currents from cell to cell forming a functional syncytium
- :. 100s of cells are depolarised and contract at the same time
- single unit smooth muscle as opposed to multiunit smooth muscle

How does electrical activity start and spread through muscle cells?
Spontaneous activity across the synctium is driven by specialised pacemaker cells.
It is modulated by:
- intrinsic (enteric) and extrinsic (autonomic) nerves
- numerous hormones
In the
- stomach
- small intestine
- large intestine
spontaneous activity occurs as slow waves- rhythmic patterns of membrane depolarisation and repolarisation that spread from cell to cell via gap junctions .
What is the role of slow wave activity in the GI tract?
Determines the max.
- frequency
- direction
- velocity
of rhythmic contractions
How does slow wave electrical activity work?
It’s driven by interstitial cells of Cajal (ICCs)
- pacemaker cells interspersed between SMCs
- located between the longitudnal and circular muscle layers and in the submucosa
- ICCs form gap junctions with each other and smooth muscle cells
Contraction only occurs is the slow wave amplitude is sufficient to trigger SMC action potentials
- upstroke is mediated by voltage-activated Ca channels; downstroke by voltage-activated K channels
- force is related to number of action potentials discharged
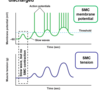
What is the basic electrical rhythm?
Slow waces determine the basic electrical rhythm
- BER varies along the length of the GI tract
- stomach: 3 slow waves per minute
- small intestine: aprox. 12 wav/min in duodenum; aprox. 8 wav/min in terminal ileum
- large intestine: aprox. 8 and 16 wav/min in proximal & distal colon respectively; favours retention of luminal contents facilitating reabsorption of water and electrolytes
- not all slow waves trigger contraction
What is the enteric nervous system?
Aprox. 100mil neurones, cell bodies mostly located in ganglia connected by fibre tracts within:
- myenteric (Auberbach’s) plexus
- mainly regulates motility and sphincters
- submucous (Meissner’s) plexus
- mainly modulates epithelia and blood vessels
Describe the enteric nervous system in relation to the GI system.
The ENS is intrinsic to G.I tissue
- reflex circuits can operate independently, but hormones and extrinsic nerves exert a strong regulatory influence
It co-ordinates muscular, secretive and absorptive activities via:
-
sensory neurones
- mechanoreceptors, chemoreceptors, thermoreceptors
-
interneurones
- the majority, co-ordinating reflexes and motor programs
-
effector neurones
- excitatory and inhibitory motor neurones supplying both smooth muscle layers, secretory epithelium, endocrine cells and blood vessels
Explain how and what effects parasympathetic innervation of the GI tract happens/causes
Pre-ganglionic fibres (releasing ACh) synapse with ganglion cells (in essence post-ganglionic neurones) within the ENS
Excitatory Influences:
- increase gastric, pancreatic and small intestinal secretion,
- blood flow and
- smooth muscle contraction
Inhibitory Influences:
- relaxation of some sphincters,
- receptive relaxation of stomach

Explain how and what the sympathetic innervation happens/causes.
Pre-ganglionic fibres (releasing ACh) synapse in the prevertebral ganglia. Postganglionic fibres (releasing NA) innervate mainly enteric neurones, but also other structures
Excitatory Influences
- increased sphincter tone
Inhibitory Influences
- decreased motility, secretion and blood flow

What role do local, short and long reflexes play in the function of the GI tract?
They modulate motor and secretory function
- Local reflex
- peristalsis
- Short reflex
- intestino-intestinal inhibitory reflex
- local distension activates sensory neurones exciting sympathetic pre-ganglionic fibres that cause inhibition of muscle activity in adjacent areas
- intestino-intestinal inhibitory reflex
- Long reflex
- gastroileal reflex
- increase in gastric activity causes increased propulsive activity in the terminal ilieum
- gastroileal reflex

What are the major motility patterns in the GI Tract?
- Peristalsis
- Segmentation
- Colonic Mass Movement
- Migrating Motor Complex (MMC)
- Tonic Contraction
Define peristalsis
‘a wave of relaxation, followed by contraction, that normally proceeds along the gut in an aboral direction- triggered by distension of the gut wall’
How does peristalsis occur in the GI Tract?
(should be able to figure this out from other info)

Describe segmentation
- one of the major motility patterns in the GI tract
- mixing or churning movements
- rhythmic contractions of the circular muscle layer that mix and divide luminal contents
- occurs in small intestine (in fed state) and in the large intestine where it is called haustration)
Describe colonic mass movement
- one of the major motility patterns
- powerful sweeping contraction that forces faeces into the rectum
- occurs a few times a day
Describe migrating motor complex (MMC)
- one of the major motility patterns
- powerful sweeping contraction that stomach to terminal ileum
Describe tonic contractions
- one of the major motility patterns in the GI tract
- sustained contractions
- low pressure- organs with a major storage function (e.g. stomach)
- high pressure- spincters
What are the locations of the major sphincters within the GI tract?
- Upper oesophageal sphincter (UOS)
- Lower oesophageal sphincter (LOS)
- Pyloric sphincter
- Ileocaecal valve
- Internal and external anal sphincters
What are the functions of the UOS?
skeletal muscle
- relaxes to allow swallowing
- closes during inspiration
*Upper Oesophageal Sphincter*
What are the functions of the LOS?
- relaxes to permit entry of food to the stomach
- closes to prevent reflux of gastric contents to the oesophagus
*Lower Oesophageal Sphincter*
What are the functions of the pyloric sphincter?
- regulates gastric emptying
- usually prevents duodenal gastric reflux
Describe the functions of the ileocaecal valve
regulates flow from ileum to caecum
- distension of ileum opens, distension of proximal colon closes
Describe the functions of the internal and external anal sphincters.
NB!!!!! Internal: smooth muscle and External: skeletal muscle
- regulated by the defaecation reflex
Outline the gross anatomy of the stomach.
- J-shaped bag
- relaxes receptively to accomodate food from oesophagus
- 50-1000ml capacity
Outline the mechanical function of the stomach
- mixes food with gastric secretions to produce semi-liquid called chyme
- stores food before passing it into small intestine as chyme
- limited amount of absorption
Relate the anatomical areas of the stomach to their functional role.
Fundus
- next to oesophagus
- thin smooth muscle layer
- receives food but little mixing
- little food stored here- usually gas
Body
- middle section
- thin smooth muscle layer
- little mixing
- food stored here
Antrum
- next to duodenum
- thicker smooth muscle layer
- highly contractile
- much mixing of chyme 30ml at a time with gastric secretions
What are the two spincters in stomach?
Lower oesophageal
Pyloric sphincter

What are the 5 cells found in gastric glands?
And in which areas are the 5 cells found?
- D cell; somatostatin (Pyloric gland area)
- G cell; gastrin (Pyloric gland area)
- Chief cell; pepsinogen (Oxyntic mucosa)
- Parietal cell, HCl, intrinsic factor gastroferrin (Pxyntic mucosa
- Enterochromaffin-like cell; histamine (Oxyntic mucosa)

What are the 7 gastric secretions and their functions?
- HCl
- activates pepsinogen to pepsin
- denatures protein
- kills most (not all) micro-organisms ingested with food
- Pepsinogen
- inactive precursor of the peptidase, pepsin. Note: pepsin once formed activates pepsinogen (autocatalytic)
- Intrinsic factor and gastroferrin
- bind vitamin B12 and Fe2+ respectively, facilitating subsequent absorption
- Histamine
- stimulates HCl secretion
- Mucus
- protective
- Gastrin
- stimulates HCl secretion
- Somatostatin
- inhibits HCl secretion
What is a secretagogue? Give important examples
A substance that causes another substance to be secreted.
- ACh
- gastrin
- histamine
How is gastric secretion controlled?
Stimulatory and inhibitory mechanisms that occur in three overlapping phases.
-
Cephalic Phase
- before food reaches the stomach preparing stomach to recieve food
- ‘in the head’
- driven directly & indirectly by CNS and vagus nerves
-
Gastric Phase
- when food is in stomach
- involves both physical and chemical mechanisms
-
Intestinal Phase
- after food has left stomach
- chyme entering the upper small intestine causes weak stimulation of gastric sectin via neuronal and hormonal mechanisms
CGI
How is gastric acid secretion inhibited?
Involves cephalic, gastric and intestinal phases.
-
Cephalic Phase
- __vagal nerve activity decrease upon cessation of eating and following stomach emptying
-
Gastric Phase
- __antral pH falls when food exits stomach (due to decreased buffering of gastric HCl)- release of somatostatin from D cells recommences, decreasing gastrin secretion
- prostaglandin E2 (PGE2) continually secreted by the gastric mucosa acts locally to reduce histamine- and gastrin- mediated HCl secretion
-
Intestinal Phase
- __the factors that reduce gastric motility also reduce gastric secretion (e.g. neuronal reflexes, enterogastrones)
What are the four main drug classes that influence acid secretion?
-
Muscarinic receptor antagonists
- block competitively
-
Proton-pump inhibitors
- block by covalent modification
- e.g. omeprazole
-
H2 histamine receptor antagonists
- block competitively
- e.g. ranitidine
- NSAIDs
- block IRREVERSIBLY
- e.g. ASPIRIN
How does the body naturally protect its mucosa from attack by HCl and pepsin?
Locally produced PROSTAGLANDINS (PGE2 and PGI2):
- reduce acid secretion
- increase mucus and bicarbonate secretion
- increase mucosal blood flow

Mankind has created drugs that reduce gastric acid secretion. What are these drugs used to treat?
Peptic Ulcer
GORD
Acid Hypersecretion
- GORD= Gastro-oesophageal reflux disease
- inappropriate relaxation of lower oesophageal sphincter allowing reflux of acid gastric contents tino oesophagus and subsequent tissue damage- oesophagitis
- Examples of acid hypersecretion
- Zollinger-Ellison syndrome
- a rare, gastrin-producing, tumour
- Cushing’s ulcers
- hieghtened vagal tone
- Zollinger-Ellison syndrome
What are the different mechanisms of different anti gastric acid secretion drugs?
Mechanisms of anti-secretory activity include:
- irreversible inhibition of the proton-pump (H+/ K+ ATPase)
- competitive antagonism of histamine H2 receptors
- competitive antagonism of muscarinic M1 and M3 ACh receptors (mostly obsolete)
- antagonism of gastrin (CCK2) receptros (not utilized clinically)

