Pharmacology and Therapeutics - Carie Martin Flashcards
(24 cards)
What is CKD?
A progressive and irreversible condition
Known as an eGFR of <60ml/min/1.73m2 and/or kidney damage that is present for 3 or more months
What molecule is used to measure glomerular filtration rate?
And why?
Creatinine –> A waste product from muscle
It is generated at a relatively constant rate
Mostly removed via filtration
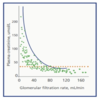
However…. Affected by age, race and weight, and it has a non-linear realtionship with true GFR
What equation is used to calculate renal function in order to figure out dosing adjustments?
And what are the downsides of this?
Cockcroft and Gault (CrCl)
Not accurate when the CrCl is less than 20ml/min
Also problematic in those with large body weight/muscle

What are some of the causes of CKD?
Diabetes –> Number 1 cause
Hypertension
Previous AKIs
Nephrotoxic drugs
Glomerulonephritis
Reflux neuropathy
What are some of the complications of CKD?
Itching –> Due to build up of toxins
Oedema
Nausea
Restless legs and cramps
Electrolyte imbalances

Can ACEi be used in CKD?
YES
They are protective in low doses
Contraindicated in AKIs!
How do we manage Renal Anaemia in CKD?
Give Erythropoiesis Stimulating Agents (ESAs) and iron (eg, Darbepoetin)
Aim for a Hb level of 10-12g/dL
How does Renal Bone Disease occur?
And how is treated?
A reduction in Vit D hydroxylation causes hypocalcemia. This increases parathyroid stimulation, which causes more calcium and phosphate to be released from our bones
Use alfacalcidol 250ng three times week (already hydroxylated vitamin D)
Phosphate binders are also used (eg, calcium carbonate/acetate)

What can Uremia cause?
Displacement of drugs from protein binding sites
Eg, phenytoin/diazepam/digoxin/sodium valproate/warfarin
What is the effect on insulin in CKD?
Insulin cannot be cleared, so its half-life is increased
So dose requirements are decreased
Which types of drugs will have problematic elimination in CKD?
Those that have over 25% excretion (unchanged) in the kidneys

Define Frailty
A syndrome of physiological decline in late life, characterised by marked vunerability to adverse health outcomes
People arent always old!!….but more likely
What’s the difference between compliance and adherence?
Compliance –> The extent to which the patients behaviour matches the prescriber’s recommendations
Adherence –> The extent to which the patients behaviour matches agreed recommendations from the prescriber
Give some examples of intentional and unintentional non-adherance
Unintentional –> Difficulty swallowing large tablets, Memory Problems, Complicated polypharmacy
Intentional –> Lack of confidence in drugs/prescriber, concerns of side effects, lack of information
What 5 things are assessed in a NOMAD assessment?
Knowledge
Visual Issues
Manual Dexterity
Cognition
Supply
Explain some PK changes that occur in the eldery
Absorption –> Reduced rate, but extent remains unchanged
Distribution –> Increased body fat and less total body water (longer half-life of fat soluble drugs, and increased serum conc of water soluble drugs)
Metabolism –> Reduced albumin (increased free drug conc of protein bound drugs) and muscle mass (increased free conc of muscle bound drugs like digoxin)
Elimination –> Predicatble age related decline in kidney function, which causes accumulation of renally excreted drugs
What monitoring must be done for somebody on digoxin?
K+ levels
Due to the possibility of hypokalaemia
What is the main aim of osteoporosis managment?
Reduce the risk of fractures (#)
Do this by correcting deficincies in vitamin D and calcium (oral bisphosphonates are first line)
How is osteoporosis diagnosed?
A DXA assessment, with a T-score of -2.5 SD
If clincically unsuitable, and over 75, the clinican can assume diagnosis without this assessment
What are the levels of calcium and vitamin D that need to be prescribed in the following patients…
Calcium intake is adequate
Inadequate calcium intake
Inadequate calcium intake plus housebond
Adequate intake –> 400units of Vit D
Inadequate –> 400units of Vit D plus 1000mg of calcium OD
Inadequate plus housebound –> 800units of Vit D plus 1000mg of calcium OD
When can denosumab be used in osteoporosis?
Secondary prevention of fractures in postmenopausal women who are unable to take alendronate and either riseondronate or etidronate
What is the impact of falls in patients?
Fractures
Confusion
Loss of confidence (psychological problems)
Soft tissue injuries
What are the 2 classes of drugs that provide the biggest risk of falls?
Drugs acting on the brain (psychotropic drugs)
Drugs acting on the heart and circulatory system

When will people be refered to a falls clinic?
If they have frequent falls
Poor balance
Undiagnosed dizziness
Syncope (unknown cause)


