Physiology 1 22 Flashcards
(136 cards)
There are two components to respiration what are they ?

The two compenents of respiration = Internal and External
External respiration = external environment to tissue
- Ventilation = bulk transport of external media across a gas exchange surface
- respiratory exchange - diffusion
- circulation
- cellular exchange
Internal respiration = cellular metabolism

What is Dalton’s law ?
Daltons law
- the partial pressue of gas
- the total pressure of a gas is equal to the sum of the partial pressures of the individual gases in a mixture
With altitude as the total pressure decreases, the partial pressure of a particular gas will decrease.
Partial pressure of oxygen = PO2
The partial pressure of any gas will change with environment.
What is Henry’s law ?
Henrys law
The amount of gas dissolved in a liquid is afftected by the gases partial pressure and solubility coefficient of that gas.
gas dissolved = pressure of gas in the media * solubility coefficient
- gas and liquid are in equilibrium
- only free gas molecules (physically dissolved contribute to the partial pressure of gas in liquid)
- gases will always diffuse down their partial pressure gradients.

What is Fick’s law, and what four factors affect the rate of diffusion ?
Describes the net diffusion rate of a gas across a fluid membrane.
- gases move down their partial pressure across a semi permeable membrane
Rate of diffusion
- surface area
- thickness or distance (T)
- pressure gradient (P)
- Diffusion coefficient (D)
What is Boyle’s law ?
Boyle’s law
For a fixed amount of an ideal gas kept at a fixed temperature, pressure and volume are inversly proportional.

What is tidal breathing and flow through breathing ?

Flow through breathing
- unidirectional flow of media, yeilds greater O2 uptake
- birds, fish and some crocodiles
Tidal breathing
- relatively inefficient as external medium moves in and out through the same opening
- mammals (bidirectional).
- fresh media is mixed with depleted media

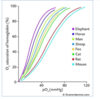
Describe concurrent, cross current and countercurrent gas exchange ?
Concurrent exchange
- external medium and blood flows in the same direction
- partial pressure gradient declines
- does not exist in a biological system
Cross current exchange
- external medium and blood travels at right angles to each other
- diffusion occurs through-out declines gradually
- PO2 is higher in blood then external medium at the end
- birds
Coutercurrent exchange
- external medium and blood flows in the opposite direction and parallel to each other
- partial pressure gradient is maintained and diffusiin is constant
- fish highly efficient

Describe gas exchange in fish through the use of gills ?2
Gills
- countercurrent exchange system
- flow through
- at every point O2 is diffused into blood - great efficiency in gas exchange
- four gill arches - filaments - lamella
- large surface area which is proportional to how active the fish is
Buccal pressure pump - fish opens and closes mouth
Opercular suction pump - fish open and close opercular flaps

Describe the upper and lower respiratory tract, what are these systems purpose?

Upper respiratory tract
- located outside the chest cavity
- no gas exchange anatomical deadspace
- covered with mucus and ciliated epithelium
- trachea and bronchi supported by cartilage
- smooth muscle lines trachea, bronchi and bronchioles.
Function = conditioning of air (warm, humidification), and filtration muco-ciliary escalator
Lower respiratory tract
- alveolar surface thin layer of squamous epithelial cells (type one)
Contains three cell types
- Type one alveolar cell - assist in gas exchange
- Type two - large cuboidal produce surfactant
- Alveolar macrophage - phagocytic patrol the alveolar surface.

Hoe does air move into the lungs ?
By creating negative pressure. Increasing volume by contraction of the diaphragm and external intercostal muscles.
Describe the histological sections of the upper respiratory tract ?
Trachea = C shaped cartilage
Bronchi = cartiliginous plates
Bronchioles do not have cartilage
The amount of smooth muscle increase from the trachea to the bronchioles.

Describe the histology of the alveolar ?
Alveolar
- Alveolar surface covered by a dense capillary surface, lung interstitium has mast cells, connective tissue and elastic tissues to hold the alveolar open.
- mainly composed of type one alveolar cells - single layer of a single layer of sqaumous epithelial cells.
- Type two alveolar cells are cuboidal and secrete surfactant and the fluid layer which lines the lungs
- Alveolar macrophage

What effect does the parasympathetic and sympathetic nervous system have on the lungs ?
Sympathetic
- air way relaxation
- blood vessel constriction
- inhibition of glandular secretion through beta 2 receptors
Parasympathetic
- air way constriction
- blood vessel dilation
- increased glandular secretion
- vagus nerve

Describe the intrapleural space and the intrapleural pressure, and what they do?

Intrapleural space
- pleura anatomically seperates the lungs from the thoracic wall
- enables friction free movement between the lungs and the thorax
- lung is mechanically connected to the thoracic cage and pleura by the pleural fluid
- pressure of fluid is negative (intrathoracic pressure) holds the lungs open
- -3mmhg
- intrapleural space of the two lungs is seperated in most species
- cause for negativity is the mechanical interaction between the lungs and chest wall.
During quiet inspiration the intrapleural pressure becomes more negative, while during expiration it becomes less negative.

What is the intrapulmonary pressure (Palv) ?
Alveolar or intrapulmonary pressure is the pressure of the air inside the lung alveoli
Normal respiration alveolar pressure decreases to about -1 mmhg (inspiration) and rises to about 1mmhg during expiration.

What is the transpulmonary pressure ?
Transpulmonary pressure
Is the difference between the alveolar pressure and the pleural pressure (distending pressure)
- the more positive the distending pressure ptp becomes the more the lungs are distended or inflated
- ptp= Palv -Ppl

Describe Pulmonary ventilation in mammals ?
Inspiration
- diaphragm and intercostal muscles contract
- lung volume increases
- lung pressure decreases belwo atmospheric pressure
- air flows down its concentration gradient
- inspiration is always active as it requires muscle contraction
- 1-2% of the total energy metabolism
Expiration
- diaphragm and intercostal muscles recoil
- lung volume decreases
- lung pressure increases
- internal intercostal muscles may contract to assist with expiration
- passive process in rest

What is eupnea ?
normal quiet breathing
What is Hyperpnea ?
increased depth and frequency of breathing during exercise
What is Tachypnea ?
excessive rapidity of breathing
What is bradypnea ?
abnormal slowness of breathing
What is polypnea ?
rapid shallow breathing, as occurs during panting
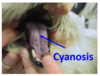
What is dyspnea ?
Difficult, painful or laboured breathing - pathological
What is apnea ?
cessation of breathing, in clinic refers to transient state of cessation of breathing