Physiology of the Heart Flashcards
(238 cards)
List the transportation roles of the heart and circulation
Transporting:
- Vitamins
- Nutrients
- Oxygen/CO2
- Hormones
- Immunoglobulins
- RBC/WBCs
Give the thermoregulatory roles of the heart and circulation
- Counter-current exchange mechanism
- Circulation of the skin
Give the 3 major parts of the circulation
- Heart
- Systemic circulation
- Lung circulation
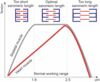
Describe Starling’s effect
To increase load, the heart automatically reacts with extra work
without hormonal/neuronal factors
Describe the heart’s work load status during rest
The heart is working in the lower range of its total working capacities
This is ensured by parasympathetic predominance
A decrease of parasympathetic activity may cause…
An increase in the mechanical performance of the heart
The autonomity of the heart rythmn is due to…
Rythmn generators in the SA node
Give the main parameter of cardiac mechanical performance
Cardiac output
The volume of blood propelled into the aorta from the left ventricle per unit time
List the layers of the heart
- Endocardium
- Myocardium
- Epicardium
- Pericardium
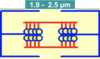
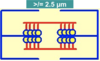
Give the contractile components of the myocardium
- Heart muscle fibres (working fibres)
- Stretching enhances their force-generating capability
Give the non-contractile components of the myocardium
- Serially attached elastic elements (SEC)
- Parallelly attached elastic elements (PEC)
- Collagen
List the functions of the pericardium
- Fixation: keeps the heart in the mediastinum
- Protection from infection from other organs
- Prevents excessive dilation of the heart during hypervolemia
- Lubricates the heart
Describe fetal circulation in relation to the pulmonary circulation
- Lungs not functioning
- Blood bypasses lungs → foramen ovale
- Between L & R atrium
Describe the closing of foramen ovale
- Pressure in left atrium increases
- Flap valve covers foramen ovale
- After 1 year, the foramen completely closes
- It is then regarded as fossa ovalis
- What percentage of the population does the foramen ovale not seal?
- What is the condition called?
- 30%
- Patent foramen ovale (PFO)
Name the fetal vessel between a. aorta thoracica and a. pulmonalis
Ductus botallo
When does ductus botallo close?
4 weeks postpartum
List the excitable varieties of cardiac tissue
- Pacemakers
- Conductive system
- Working fibres
Purpose of the Aschoff-Tawara (AV) node
Delays the atrial signal
So atrial contraction precedes the ventricular contraction
Resting membrane potential (RMP)
Diastole:
- -90mV
- Spontaneous depolarisation followed by AP
- RMP doesn’t exist in pacemaker cells
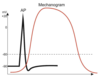
Describe action potential (AP)
- Stimulation
- _Ion channel_s of membrane open
- Ion exchange between the two sides
- Action potential
Pacemaker potentials
Pacemaker cells
- Located: SA / AV node
- Allow continuous generation of excitation
- No RMP
- Repolarisation: Transmembrane potential -55mV
- Automatic depolarisation follows
This electrical activity is expressed in…

Sinoatrial (SA) node