revision lecture Flashcards
(25 cards)
what are the key features of rheumatoid arthritis *
morning stiffness around teh joints
symetrical polyarthritis - typically involving the small joints of the hand/wrist
subcut nodules
rheumatoid factor
joint erosions on radiograph
define rheumatoid factor *
Ab that racognise the Fc portion of IgG as their target Ag
IgM targetting IgG
IgM is pentameric so get big complex
what is hyaluronic acid
a non-sulfated glycosaminoglycan
collagen type in synovium *
1
define reactive arthritis *
sterile inflamm synovitis following an infection
extra-articular manifestations - enthesopathy, skin inflammation (cricinate balanitis, keratoderma blennorrhagicum - this is psoarisis like skin lesions )
eye inflammation (conjunctivitis)
control the symptoms but patients get better over time
important to know the different features because if have all dont need to giev AB for eye - giev anti-inflamm and should get better
however - could be 1st manifestation of psoriatic arthritis, could be presentation fo ankylosing spondylitis
infections associated with reactive arthritis *
Urogenital infections
enterogenic infections
may be the 1st manifestation of HIV or Hep C infection
need to think about these for treatment
describe and give 2 examples of enthesopathy *
inflammation where a ligament, tendon, fascia or capsule insert into the bone
they are seronegative arthropathies
eg
achilles tendon - painful heel - inflamm where inserts into calcaneum - may be trauma or inflammatory arthropathy
plantar fascilitis - painful feet - inflammation at insertion of plantar fascia
dactylitis - swollen digits - inflammation at insertion of capsule and ligamnets in digits
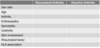
compare these featres of rheumatoid and reactive arth *

summarise the pathological finding inosteoarthritis *
irreversible loss of articular cartilage
there are focal areas of damge to articular cartilage
new bone formation at joint margins - osteophytosis
changes in subchondral bone - sclerosis
define proteoglycan *
glycoproteins containing sulfated glycosaminoglycan chains - eg aggrecan
define glycosaminoglycan *
repeating polymers of disaccharides eg
chondroitin sulphate
keratin sulphate
hyaluronic acid
what is the major collagen and proteoglycan found in articualr cartilage *
type 2 collagen
aggrecan
describe the structure and composition of articular cartilage *(
type 2 collagen
aggrecan - monomers are arranged into supramolecular aggregates consisting of central hyaluronic acid filament and non-covalently linked aggrecan
negatively charged chemical groups of GAGs attract water into cartilage - 80% of the net weight is water
compare the radiographic signs of rheumatoid arthritis and osteoarthritis *
joint space narrowing not present early in Rheum
get osteopenia around the immobile joint
list the major HLA association for
ankyloising spondylitis and reactive arthritis
SLE
rheumatoid arthritis *
ank and reactive - HLA-B27
SLE HLA-DR3
rheum HLA-DR4
summarise the composition of bone *
comprised of protein matrix (osteoid) and mineral hydroxyapatite
osteoclasts resorb bone and osteoblasts form it
define osteoporosis *
predisposition to skeletal fractures resulting from a reduction in regional or total bone mass
bone chemistry is normal - serum ca, phos, pth and alkaline phosphtase
assesed by DEXA - defined by a T score
T score is comparison of pts mean bone mass to the mean of young normal subjects - mean of young normal subjects represents ‘peak bone mass’
T score calculates how many SDs pts score is above or below the peak bone mass
get osteopenia and fragility fractures
define osteomalacia *
impaired mineralisation in mature bones, rickets is impaired mineralisation in immature bones
most frequently due to inadequate extracellular fluid conc of phosphate or ca
causes of osteomalacia *
vit D def
abnormal vit D metabolism - eg liver or kidney disease
hypophosphtaemia - may be due to renal phosphate loss which can be determined by measureing urinary phosphate levels
what are the biochemical changes in bone diseases *

what is osteomalacia associated with *
low or normal serum ca
low phos - PTH drives phosphate out of the kidney
secondary hyperparathyroidism - high pth and serum alkaline phosphtase
osteopenia and pseudofractures eg looser ones
in rickets - flared ends of bones and bowing of long bones
define pagets *
disroder of bone remodelling of unknown cause where there is increased bone resorption followed by increased formation = disorganised mosaic of woven and lamella bone
bone chemistry shows high alkaline phosphtase
increased cortical bone thicjness on radiographs eg sclerosis
abnormal bone causes pain and bone deformity and sometimes fractures
expansion of bone
rare causes of OA *
metabolic and genetic
describe the joint in OA *
have exposed bone
joint space narrowing becaus eof lack of articular cartilage


