Soft Tissue Infection Flashcards
(34 cards)
A 30-year-old Florida fisherman comes to the emergency department 24 hours after cutting his palm with a fish-scaling knife. Blood pressure is 90/50 mmHg and heart rate is 120 bpm. Physical examination shows severe swelling of the hand, hemorrhagic bullae of the hand, and erythema to the mid forearm. X-ray study shows no gas within the soft tissues. A Gram stain of drainage from a bulla reveals gram-negative bacilli. Which of the following infectious agents is the most likely cause of the patient’s symptoms?
A) Clostridium perfringens
B) Mycobacterium marinum
C) Pseudomonas aeruginosa
D) Staphylococcus aureus
E) Vibrio vulnificus
The correct response is Option E.
The patient described has necrotizing fasciitis and sepsis. Vibrio vulnificus is a gram-negative bacillus, a cause of necrotizing fasciitis, and is commonly associated with warm saltwater environments (Florida). It also tends to present with hemorrhagic bullae. Staphylococcus aureus is a gram-positive coccus, is not associated with watery environments, and is more commonly associated with pustules rather than hemorrhagic bullae. Clostridium perfringens is a gas-forming, gram-positive bacillus, and is associated with marine sediment. Pseudomonas aeruginosa, also a gram-negative bacillus, although associated with moist environments, is more typically associated with less aggressive soft-tissue infections. Mycobacterium marinum is also associated with watery environments, but tends to affect aquarium owners with an indolent granulomatous process.
2018
A 53-year-old woman undergoes bilateral mastectomy and autologous breast reconstruction. Four days postoperatively, the patient reports moderate abdominal discomfort and multiple episodes of diarrhea. Vital signs are within normal range. Physical examination shows a mildly distended abdomen. Stool sample is positive for Clostridium difficile toxin. Treatment with which of the following drugs is most appropriate first-line treatment in this patient?
A) Fidaxomicin
B) Metronidazole
C) Rifaximin
D) Teicoplanin
E) Vancomycin
The correct response is Option B.
Oral metronidazole is the most appropriate treatment for this patient with a mild/moderate form of Clostridium difficile infection.
Oral vancomycin is recommended for treatment of those with severe disease, or with mild/moderate disease who did not respond to metronidazole.
Patients who cannot tolerate oral medications (eg, postoperative ileus) or who have an intestinal diversion (eg, ileostomy) can be treated with intravenous metronidazole or with vancomycin enemas. Vancomycin is not excreted into the colon and therefore should not be given intravenously to treat C. difficile infection.
Oral fidaxomicin has been shown to be as effective as oral vancomycin in the treatment of C. difficile infections. Although further clinical experience is still needed, this drug has been associated with increased cure rate in patients receiving concomitant antibiotics and decreased infection recurrence when compared to vancomycin.
Teicoplanin and rifaximin are not generally recommended for treatment of C. difficile, although isolated reports of successful therapy can be found in the literature.
2018
Which of the following time frames for onset most accurately reflects the CDC’s definition of surgical site infection?
A) Within 3 days of surgery or within 30 days of prosthetic implant placement
B) Within 7 days of surgery or within 3 months of prosthetic implant placement
C) Within 14 days of surgery or within 6 months of prosthetic implant placement
D) Within 21 days of surgery or within 9 months of prosthetic implant placement
E) Within 30 days of surgery or within 1 year of prosthetic implant placement
The correct response is Option E.
The CDC defines a surgical site infection as an infection that occurs at the incision site or within the organ or space operated on within 30 days after surgery or within 1 year if a prosthetic implant is placed. Infection requires at least one of the following:
Purulent drainage from the surgical site
Organisms isolated from an aseptically obtained culture of fluid or tissue at the surgical site
Spontaneous dehiscence of a deep incision or deliberate opening of the incision by a surgeon when the patient has at least one of the following signs or symptoms: fever (greater than 100.4°F [38.0°C]), localized pain or tenderness, localized swelling, redness, or heat, unless site is culture-negative
An abscess or other evidence of infection involving the incision or operative site that is found on direct examination, during reoperation, or by histopathologic or radiologic examination
Diagnosis of a surgical site infection by a surgeon or attending physician
2018
A 30-year-old man with AIDS is evaluated for a 6-week history of painless but increasing swelling of the flexor surfaces of the right wrist. Physical examination shows limited motion of the wrist and positive Phalen and Tinel signs. At the time of surgical exploration, rice bodies are present in the flexor tenosynovium. Which of the following is the most likely diagnosis in this patient?
A) Aspergillus fumigatus
B) Mycobacterium tuberculosis
C) Nocardia asteroides
D) Sporothrix schenckii
E) Vibrio vulnificus
The correct response is Option B.
Rice bodies are pathognomonic for tuberculosis.
Ziehl-Neelsen staining confirms the presence of acid-fast bacilli. All Mycobacterium and Nocardia species are potentially acid-fast. Many of these organisms are fastidious, so false-negative results are common. Surgeons should obtain multiple tissue samples and alert the laboratory that a diagnosis of tuberculosis is suspected. M. tuberculosis is traditionally cultured in Löwenstein-Jensen culture medium under specific temperature conditions 37.0°C (98.6°F). Histologic examination of specimens shows a granulomatous inflammatory process with the central portion of the granulomas appearing caseated.
If a mycobacterial infection is suspected, a Mantoux test should be performed. The test involves purified protein derivative injection into the dermis and evaluation of the cutaneous site after 48 to 72 hours.
M. tuberculosis should be considered in all immunocompromised patients. The other organisms can all be seen in hand infections in immunocompromised patients but do not produce rice bodies.
2017
A 28-year-old, right-hand–dominant woman is brought to the emergency department 18 hours after sustaining a cat bite to the dorsum of the hand proximal to the fifth metacarpophalangeal (MCP) joint. Which of the following organisms is most likely to be cultured from this abscess?
A) Eikenella corrodens
B) Group A Streptococcus
C) Methicillin-resistant Staphylococcus aureus
D) Pasteurella multocida
E) Pseudomonas aeruginosa
The correct response is Option D.
Pasteurella multocida is a small, gram-negative coccobacillus that is frequently associated with infections caused by dog and/or cat bites. Local findings are consistent with infection including erythema, warmth, pain and tenderness, and fluctuance or purulent discharge. Delayed treatment may result in chronic deep-space infection and/or osteomyelitis. Treatment involves starting penicillin combined with local wound care as well as surgical incision and debridement if needed.
Methicillin-resistant Staphylococcus aureus (MRSA) is becoming more common in community-acquired hand infections, but is not typically associated with dog or cat bites. Eikenella corrodens is more commonly associated with infections occurring after human bites. Pseudomonas infection is often seen as a nosocomial infection that is very resistant to antibiotics. Group A Streptococcus is a common bacterial infection associated with strep throat.
2017
A healthy 5-year-old boy is evaluated after he is bitten on the hand by a dog. He has an allergy to penicillin. Which of the following prophylactic antibiotic regimens is most appropriate to prescribe?
A) Amoxicillin and clindamycin
B) Ciprofloxacin and metronidazole
C) Clindamycin only
D) Doxycycline and metronidazole
E) Trimethoprim-sulfamethoxazole and clindamycin
The correct response is Option E.
The most appropriate prophylactic regimen to prescribe in this clinical scenario is trimethoprim-sulfamethoxazole and clindamycin.
Dog bites to the hand are potentially dangerous bites that could lead to serious hand infections. The common microorganisms that cause infections in such bites are Pasteurella species, anaerobes, Staphylococcus aureus, and Streptococcus. The ideal antibiotic would have been amoxicillin-clavulanic acid, which covers most of these microorganisms. However, the child is allergic to penicillin, and, therefore, this drug is contraindicated. Another good option would have been amoxicillin and clindamycin (for the anaerobic coverage). However, for the same reason described above, it too cannot be used. Tetracyclines are contraindicated in children under 8 years of age owing to the ill effects on growing teeth and bones. Quinolones are also contraindicated in children under 18 years of age owing to their harmful effects on cartilage and joints. Although this is debatable, currently the use of quinolones in children is restricted by the Food and Drug Administration to certain specific conditions (cystic fibrosis, multidrug-resistant urinary tract infection, and inhalational anthrax). Clindamycin alone does not adequately cover most of the organisms involved, including Pasteurella, which is gram-negative.
2016
A 34-year-old woman comes to the emergency department 5 days after sustaining a cat bite to the left index finger. A photograph is shown. Medical history includes diabetes mellitus type 1. Physical examination shows punctures to the dorsum and volar surfaces of the proximal phalanx, mild fusiform swelling of the digit with tenderness over the flexor tendon sheath, pain with passive extension, and partially flexed posture of the digit. The symptoms have worsened over the past 3 days. Temperature is 99°F (37.2°C). Which of the following is the most appropriate next step in management?
A) Incision and drainage of the puncture sites
B) Inpatient intravenous antibiotics
C) Irrigation of the flexor sheath
D) Outpatient oral antibiotics
E) Splinting immobilization and elevation

The correct response is Option C.
The most appropriate option for this patient is to proceed to the operating room for decompression/drainage of the flexor tendon sheath. This patient has all four of Kanavel’s signs, specifically pain on passive extension, fusiform swelling, flexor tendon sheath tenderness, and flexion of the affected digit. These point towards a diagnosis of flexor tenosynovitis, with the cause being the cat bite she sustained several days prior. Although cat bites only reflect 5% of all animal bites, they represent 76% of all infected bites, thought to be because of the morphology of their long teeth, which simulate a deep puncture wound.
Outcomes studies demonstrate that because of this patient’s diabetes, she is at risk for a poor outcome, specifically the need for amputation and/or decreased total active motion. Other risk factors that can lead to these outcomes include age greater than 43 years, presence of subcutaneous purulence, digital ischemia, and polymicrobial infection. Given that she is at risk and that she has all four Kanavel’s signs, any intervention that is more conservative than operative decompression and drainage may lead to suboptimal outcomes.
Administration of antibiotics (orally or intravenously) is not a substitute for drainage of the flexor sheath, especially in a case that presents more than 48 hours out from initiation of symptoms. Drainage in the emergency department is not as optimal as in the operating room given that the infection may limit efficacy of local anesthesia as well as the need for possible conversion to an open drainage procedure if closed catheter irrigation is insufficient.
2016

A 60-year-old woman who works as a nurse in the intensive care unit (ICU) is scheduled for cardiac bypass surgery. Because she has taken care of many patients with methicillin-resistant Staphylococcus aureus infection, she is interested in topical agents for decolonization. Which of the following regimens is most appropriate for this patient?
A) Clindamycin
B) Linezolid
C) Mupirocin and chlorhexidine
D) Trimethoprim-sulfamethoxazole
E) Vancomycin
The correct response is Option C.
The currently accepted decolonization protocol from the Infectious Diseases Society of America is a combination of topical nasal mupirocin ointment and a chlorhexidine body wash for 5 days. The most robust data for decolonization are in the cardiac surgery literature; the Society of Thoracic Surgeons guidelines recommend routine prophylaxis for all patients undergoing cardiac surgery. These guidelines are based on studies that show a decreased rate of sternal wound infections.
The carriage rate of methicillin-resistant Staphylococcus aureus for health care workers is approximately 5% based on large review studies. As a substantial portion of cases originate from nasal colonization, routine screening and decolonization are recommended in areas where the carriage rate exceeds 10% (Centers for Disease Control and Prevention recommendation).
The other antibiotics listed are reserved for the treatment of infection rather than as part of a decontamination protocol.
2016
Which of the following antibiotics is most effective in decreasing Staphylococcus aureus infections in irradiated wounds?
A) Cefazolin
B) Doxycycline
C) Nafcillin
D) Trimethoprim-sulfamethoxazole
The correct response is Option D.
The prophylactic use of trimethoprim/sufamethoxazole (TMP/SMZ) in irradiated wounds, primarily in the setting of implant-based breast reconstruction, has been shown to reduce the rate of skin-derived infections. Mirzabeigi et al1 reported a 28% reduction in infection rates with the use of TMP/SMZ when compared with cephalosporins, in an irradiated chest wall wound. Based on their data, the authors advocate a monthlong prophylactic course of TMP/SMZ to reduce infection rates in this high-risk population. This is likely due to the ability of TMP/SMZ to treat both methicillin-resistant Staphylococcus aureus (MRSA) and Staphylococcus epidermidis. This has been supported by other published reports.2,3
Cefazolin and nafcillin do not effectively treat MRSA, reducing their clinical ability to prevent skin-related infections in this high-risk population. Doxycyline has some efficacy in treating most skin flora, including MRSA, but there is no clinical evidence to suggest it outperforms TMP/SMZ.
2016
A 15-year-old girl has two draining nodules of axillary hidradenitis suppurativa. Each lesion is approximately 10 mm in diameter. The remaining axillary skin shows no abnormalities. After a 6-week course of oral doxycycline and topical mupirocin, the lesions drain less but are still present. Which of the following is the most appropriate treatment for this patient?
A) Complete axillary excision and skin grafting
B) Excision and closure
C) Incision and drainage
D) Intravenous antibiotics
E) Kenalog injection
The correct response is Option B.
This young patient has limited, focal disease that has failed medical management. Local excision is useful for isolated, scattered individual, or linear lesions. More extensive disease that occupies a significant portion of the skin area may be better treated by complete axillary excision. In this younger patient with limited disease, direct excision of the affected areas is a less morbid approach. Negative pressure wound therapy and skin grafts may be optimal coverage treatments for extensive disease, and some local flaps have been described as well. This stubborn disease originates from the apocrine glands and can often be chronic and disabling. The axillae, groin, perineum, and submammary areas can all be affected. Initial treatments include local care, antibiotics, hygiene, and weight loss. Steroid injections may help in early, small lesions, but have limited effectiveness and are painful. After a 6-week course of antibiotics, this patient is not likely to benefit from more treatment. Only excision of the diseased apocrine glands is likely to be effective. Incision and drainage is a suitable treatment for a closed abscess associated with hidradenitis, but incising this patient’s lesions would not improve her situation.
2016
An otherwise healthy 10-year-old girl is brought for evaluation because of a chronic ulcer of the right leg. The ulcer first appeared 6 months ago when she scraped her leg on a boat dock at her family’s lake house. The wound has increased in size despite treatment with a course of oral antibiotic therapy prescribed by her primary care physician. A photograph is shown. On evaluation today, the patient is afebrile and has no systemic signs of infection. Which of the following organisms is the most likely cause of these findings?
A) Candida tropicalis
B) Group A beta-hemolytic Streptococcus
C) Methicillin-resistant Staphylococcus aureus
D) Mycobacterium marinum
E) Vibrio vulnificus

The correct response is Option D.
The history and presentation are classic for an atypical mycobacterial infection. Unlike bacterial infections, atypical mycobacteria rarely produce systemic signs of infection and often manifest as a nonhealing (sometimes progressive) wound. Given the history of injury on a boat dock, the most likely causative organism is Mycobacterium marinum, an acid-fast bacillus that lives in water environments. This pathogen results in localized granulomas such as the one seen in this patient. Staphylococcus aureus is the most common source of skin infections but typically results in a more pronounced and acute immune reaction with localized redness and purulence. These findings are not present in this patient. Cutaneous infections with Group A beta-hemolytic Streptococcus and Vibrio vulnificus tend to increase rapidly and are often accompanied by severe systemic response (i.e., necrotizing fasciitis). Candida tropicalis is a fungus that is often part of normal skin flora. It is related to Candida albicans and can produce opportunistic internal infections in susceptible individuals.
2016
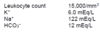
A 46-year-old woman comes to the emergency department because of a 5-day history of profound physical deterioration, nausea, and vomiting. She underwent breast reconstruction 3 weeks ago. Medical history includes delayed right latissimus dorsi tissue expansion breast reconstruction 1 year after completing radiation therapy. She has no other comorbidities. Physical examination shows erythematous rash involving and extending beyond the surgical sites. There are no notable fluid collections and the surgical wounds are not draining. Temperature is 103.5°F (39.7°C) and blood pressure is 90/50 mmHg. Laboratory studies show:
Intraoperative cultures of the explored surgical sites are most likely to grow which of the following organisms?
A) Bacteroides
B) Clostridium
C) Enterobacter
D) Pseudomonas
E) Streptococcus
The correct response is Option E.
The Centers for Disease Control and Prevention support criteria indicate that toxic shock syndrome may be diagnosed when patients present with a temperature exceeding 102°F (38.9°C), multisystems organ failure, rash, and/or multiple constitution symptoms.
Exotoxin1 and exfoliative toxin-producing Staphylococcus aureus are the most common pathogen, but enterotoxin A, B, and C, producing Streptococcus pyogenes infections, yield a worse prognosis. Blood cultures may be negative for the causitive organism.
Although Clostridium, Enterobactor, Pseudomonas, and Bacteroides species are polymicrobial species associated with necrotozing fasciitis, the description of this otherwise healthy patient is not consistent with its typical presentation of discolored blistered skin and crepitus.
2016
A 45-year-old man is brought to the emergency department with a Gustilo IIIB tibial fracture that he sustained falling off a tractor in a pasture. Medical history shows no drug allergies. Administration of which of the following antibiotics is most appropriate in this patient?
A) Amoxicillin
B) Ceftriaxone
C) Ciprofloxacin
D) Clindamycin
E) Vancomycin
The correct response is Option B.
The most appropriate antibiotic prophylaxis for this patient with a Gustilo grade III fracture is a third generation cephalosporin. Although much debate exists regarding antibiotic prophylaxis in open tibial fractures, it is generally accepted that antibiotic prophylaxis reduces the rate of infection. When antibiotic prophylaxis is not used, infection occurs in approximately 24% of open fractures. Thus, selecting the appropriate antibiotic, as well as duration, is of utmost importance. Antibiotic prophylaxis should be administered as soon as possible after injury and should be limited to a 72-hour course. In general, broad-spectrum antibiotics and multiple antibiotics should be avoided because they have been shown to increase the risk of nosocomial infections, including pneumonia. Of the antibiotics listed, the most appropriate choice for a patient with no drug allergies is ceftriaxone. Clindamycin and vancomycin should be reserved for cases of true penicillin allergy. Ciprofloxacin alone has been shown to be inferior to prevent infection after open tibial fractures.
2016
A 29-year-old woman is evaluated because of a 2.5-year history of painful, draining lesions from the axillae and groin. Physical examination shows multiple nodules and abscesses. Conservative treatment with loose clothing, topical antibiotics, and antibacterial washes is unsuccessful. These findings are most consistent with which of the following disease processes?
A) Candidal infection of the intertriginous areas
B) Follicular occlusion of the apocrine sweat gland areas
C) Follicular occlusion of the eccrine sweat glands areas
D) Inflammatory and ulcerative skin condition mediated by neutrophils
E) Sexually transmitted infection caused by Klebsiella granulomatis
The correct response is Option B.
Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic inflammatory disease of the skin and subcutaneous structures. Initially presenting as tender, subcutaneous nodules, the disease can advance to cause abscesses and large areas of subcutaneous scarring and draining sinus tracts.
Historically, HS has been thought to originate from the apocrine sweat glands. However, research in recent years has demonstrated that the mechanism is one of follicular occlusion: hair follicles become occluded due to an overproliferation of ductal keratinocytes, rupture, and subsequently re-epithelialize. As this cycle continues, sinus tracts form that house bacteria and cause chronic, painful infections and inflammation that can involve the skin and subcutaneous structures including muscle, fascia, and lymph nodes.
HS lesions typically occur predominately in the apocrine-gland bearing areas of the axillary, inguinal, perianal, and perineal areas. Lesions typically correspond with the “milk-line” pattern of apocrine-related mammary tissue in mammals.
Eccrine, or merocrine, sweat glands are found throughout the body, but their highest concentrations are in the palms and soles. These areas are typically spared by HS.
Follicular pyodermas, including folliculitis, furuncles, and carbuncles, arise primarily from the infection of hair follicles. They do not cause the sinus tracts, comedones, and scarring caused by HS.
Granuloma inguinale is a sexually transmitted infection of the genitalia, perineum, and/or perineal area caused by Klebsiella granulomatis.
Pyoderma gangrenosum is a dermatologic condition mediated by neutrophils that causes skin ulceration and breakdown.
2016
A 5-year-old boy is brought to the emergency department after sustaining a traumatic amputation of the right thumb. Medical history includes an allergy to sulfa drugs. The thumb is successfully replanted, and the patient is admitted for observation. Twenty-four hours postoperatively, venous congestion of the replanted thumb is noted. Leeches are placed to improve congestion. It is suspected that the leeches will be required for several days until venous outflow is reestablished. Administration of which of the following antibiotics is most appropriate?
A) Cefotaxime
B) Ciprofloxacin
C) Clindamycin
D) Tetracycline
E) Trimethoprim-sulfamethoxazole
The correct response is Option A.
Medicinal leeches are still commonly used as an adjunct in the treatment of venous congestion. They secrete a powerful anticoagulant called hirudin that promotes bleeding in the congested tissues until venous outflow can be reestablished. Leeches are also known to harbor the gram-negative bacterium Aeromonas. Because leeches can be exposed to open wounds on the patient for several days during treatment, antibiotic prophylaxis against Aeromonas is recommended.
Ciprofloxacin, tetracycline, trimethoprim-sulfamethoxazole (Bactrim), and third-generation cephalosporins have all been shown to be effective against Aeromonas. However, in the scenario above, all of these antibiotics have a contraindication except cefotaxime, a third-generation cephalosporin.
Ciprofloxacin is contraindicated in children when a suitable alternative exists secondary to the risk of arthropathy and arthrotoxicity. Similarly, the use of tetracycline is relatively contraindicated in children owing to the potential for abnormalities with the teeth, including permanent staining and growth retardation. While Bactrim is often used in children to treat various infections, this child has an allergy to sulfa drugs and should not be given this antibiotic.
Clindamycin does not provide effective antibiotic coverage against Aeromonas.
2016
A 67-year-old man with type 1 diabetes mellitus is evaluated for full-thickness perineal burns sustained by falling onto a space heater. Forty-eight hours after admission, he has onset of fever and tachycardia. Complete blood cell count grows leukocytosis, and wound culture shows gram-negative rods consistent with Pseudomonas. Pending sensitivity report, empiric coverage is initiated. Which of the following antibiotics is clinically CONTRAINDICATED for initial therapy?
A) Ceftazidime
B) Ceftriaxone
C) Ciprofloxacin
D) Imipenem
E) Tigecycline
The correct response is Option E.
Although tigecycline has excellent coverage of most staphylococcal and many gram-negative rod infections, this tetracycline derivative is not effective against pseudomonal infections. Patients with pseudomonal sepsis benefit from double coverage. Furthermore, sensitivities to different antimicrobial agents are quite variable from one health care system to another, so providers must remain vigilant after beginning therapy and change coverage based on lack of clinical response and determination of final sensitivities. An essential component of this patient’s care would be urgent burn wound excision, after he has been resuscitated and empiric antibiotics have been initiated.
2016
A 34-year-old woman undergoes laser-assisted liposuction of the abdomen, hips, and inner and outer thighs using a tumescent technique. A total of 2500 mL of aspirate is removed. Postoperative recovery is uneventful, and the patient is discharged home the same day. She comes to the emergency department 4 days later with intense pain over the lower abdomen and flanks. Temperature is 101°F (38.3°C). Physical examination shows the skin has well-demarcated erythema, induration, and bullae forming at multiple sites. Her incisions are seeping clear, grey fluid. Which of the following is the most appropriate management?
A) Exploratory laparotomy for presumed bowel perforation
B) Intravenous administration of antibiotics and local burn care
C) Intravenous administration of antibiotics only
D) Oral administration of antibiotics
E) Surgical debridement of the involved tissue
The correct response is Option E.
Necrotizing fasciitis is a rapidly progressive soft-tissue infection characterized by necrosis of the fascia and subcutaneous fat with subsequent necrosis of the overlying skin. Although complication rates associated with liposuction are not unduly increased, infection is a major concern, and cases of prolonged inflammation, septic shock, and infections have been documented. Likewise, cases of necrotizing fasciitis following liposuction have been reported on several occasions and, according to data reported in the literature, the overall incidence of necrotizing fasciitis is equal to 0.4 per 100,000 patients.
There are two common forms that are reported: infections caused by Streptococcus pyogenes and mixed infections caused by a variety of microbes, including Escherichia coli, Proteus, Serratia, and Staphylococcus aureus. A detailed case of necrotizing fasciitis sustained by Mycobacterium chelonae after a combined procedure of liposuction and lipofilling has also been described. The progressive necrosis of the tissues typically involves the superficial fascia and the subcutaneous layer, but is limited in extension to the skin; the extent of the gangrene at the fascial layer is usually more severe and greater than at the skin level.
Necrotizing fasciitis is virtually unnoticeable in the first 48 hours with nonspecific symptoms. In the days that follow, an extensive, hardened region forms, which is often dark in the center. Severe pain and necrosis follow at the level of the infection.
Drainage of “dishwater fluid” is often pathognomonic. Metabolic changes occur, ending with respiratory distress, oliguria, acidosis, increased troponin concentrations, and sepsis. Diagnosis and treatment consist of surgical exploration and debridement that reveal necrotic, edematous, subcutaneous fat. Bacteriologic analysis of exudate, cultures, and histologic evaluation complete the diagnosis.
Early diagnosis is imperative to avoid a fatal outcome. Treatment is based on immediate and aggressive surgical debridement with combined antibiotic therapy. Because necrotizing fasciitis is a progressive, rapid infection, the wound typically is left open for a planned “second-look” operation and additional debridement if necessary. The mortality rates are increased and range up to 70% but decrease to 4.2% after immediate surgical intervention. Delay in debridement increases mortality.
2015
A 40-year-old woman with chronic hidradenitis suppurativa of the bilateral axillae is referred for surgical management after 4 years of local wound care, multiple corticosteroid injections, and oral antibiotics failed to improve her symptoms. Physical examination shows multiple inflamed nodules and draining sinuses. Photographs are shown. Which of the following treatment options is most likely to provide long-term resolution of this patient’s symptoms?
A) Axillary lymphadenectomy and coverage with a trapezius flap
B) Carbon dioxide laser and silver sulfadiazine
C) Fistulotomy and negative pressure wound therapy
D) Lesion excision and primary closure
E) Total axillary excision and skin grafting

The correct response is Option E.
(Please note that this pictorial appears in color in the online examination)
Hidradenitis is a chronic and often disabling skin condition of the apocrine glands. It results in abscesses, inflammatory nodules, and draining sinuses in the axillae, groin, perineum, and occasionally the submammary area. It affects approximately 1 in 300 people, and it is more common in women, people who smoke, and people who are overweight. The axillae are more commonly involved in women, and the perineum more commonly in men.
Early treatment centers around local wound care, oral antibiotics, corticosteroid injections, hygiene, weight loss, and smoking cessation. Decreased estrogen levels may also contribute, and disease often subsides with oral contraceptives and during pregnancy. Unresponsive or extensive disease requires surgical intervention for long-term resolution. Relapse rates are high, and healing is often slow. Although limited excision and closure of solitary lesions is an effective short-term treatment, new lesions are likely to develop. Fistulotomy alone has an unacceptably high recurrence rate.
A long-term resolution in this severely affected patient requires complete excision of the hair-bearing skin of the affected area. The large defect created needs broad skin coverage. The best options include split-thickness skin grafting or grafting with negative pressure wound therapy immobilization. Negative pressure wound therapy followed by healing by secondary intention or coverage with local flaps are additional options, though scar contractures and shoulder stiffness are risks.
Laser treatments are too superficial to treat the deeper apocrine structures. Lymphadenectomy is not necessary for a cure.
2015

A 48-year-old right-hand–dominant man with a history of cadaveric renal transplantation comes to the emergency department because of a swollen, painful left hand. A photograph is shown. He works as a crab fisherman and reports that he was bitten in the first web space by a crab 18 hours ago. He is taken to the operating room for emergent debridement. Intraoperative Gram stain shows a gram-negative, curve-shaped rod. In addition to aggressive surgical treatment, administration of which of the following antibiotics is most appropriate to treat this patient?
A) Cephalexin
B) Levofloxacin
C) Linezolid
D) Nafcillin
E) Vancomycin

The correct response is Option B.
Vibrio vulnificus is a common Vibrio species causing soft-tissue infections of the hand. Vibrio species are ubiquitous in aquatic environments including saltwater bodies. Immunocompromised hosts are at greater risk for amputation and death. The best chance for patient survival includes early diagnosis and initiation of appropriate antibiotics, as well as urgent surgical debridement for any evidence of necrotizing infection.
A broad range of antibiotics are effective against Vibrio species, including V. vulnificus. Agents effective against gram-negative rods, including quinolones, aminoglycosides, and aminopenicillins, are all effective against V. vulnificus. While all cephalosporins are effective against Vibrio species, third-generation cephalosporins are up to 130 times more potent than first- or second-generation cephalosporins. Vancomycin, nafcillin, and linezolid are all narrow-spectrum antibiotics, primarily effective against gram-positive cocci, and are not effective against Vibrio species.
2015
A 55-year-old man with a history of smoking and poorly controlled diabetes mellitus comes to the emergency department because of a 12-hour history of unilateral proptosis, impaired vision, and severe headaches. Intranasal examination shows dried crusting and black discoloration of the lateral nasal wall and turbinates. Radiology shows a 4-cm mass within the maxillary sinus that extends into the orbit. Biopsy of the mass shows nonseptate hyphae. Which of the following is the most appropriate next step in management?
A) Craniofacial resection and free flap
B) Emergent debridement of the sinuses and orbital exenteration
C) Intravenous administration of an antibiotic
D) Outpatient oral antifungal medications
E) Referral to medical oncology
The correct response is Option B.
Rhinocerebral mucormycosis is a rare opportunistic infection of the sinuses, nasal passages, oral cavity, and brain caused by saprophytic fungi. The infection can rapidly result in death. Rhinocerebral mucormycosis commonly affects individuals with diabetes and those in immunocompromised states. The diagnosis of mucormycosis is established by obtaining a biopsy specimen of the involved tissue, and frozen tissue samples should be immediately evaluated for signs of infection. Microscopic characterization of non-septate hyphae, rhizoids, columellae, sporangia, and sporangiospores helps to define genus and species within the order Mucorales. Optimal therapy requires a multidisciplinary approach that relies on prompt institution of appropriate antifungal therapy with amphotericin B (AmB), reversal of underlying predisposing conditions, and, where possible, surgical debridement of devitalized tissue. Surgery should be considered early, and if possible, emergently with the goal of removing all necrotic tissue. Repeated debridements are frequently necessary and the extent of surgery should ideally be guided by evaluation of frozen tissue sections examined histologically. In the scenario provided, orbital involvement will most likely require sacrifice of the eye.
2015
A 15-year-old girl comes to the office because of a 1-day history of infection of the right index finger. Physical examination shows the tip of the finger is tender and swollen over the pulp. There is no history of trauma. Which of the following organisms is the most likely cause of this patient’s condition?
A) Candida albicans
B) Eikenella corrodens
C) Listeria monocytogenes
D) Pasteurella multocida
E) Staphyloccus aureus
The correct response is Option E.
Staphylococcus is still the most common organism in hand infections. The most common in felons is Staphylococcus aureus. Methicillin-resistant Staphylococcus aureus community-acquired (MRSA-CA) infections are now the most predominant strain in hand infections, comprising 60% of Staphylococcus aureus infections.
Pasteurella multocida should be considered with most animal bites, although it is most common with cat bites. Eikenella corrodens is associated with human bites. There is no history of bites in this case.
Listeria monocytogenes has been reported in flexor tenosynovitis in immunocompromised patients.
Candida albicans is usually associated with chronic paronychia.
2014
A 55-year-old man undergoes microsurgical replantation of an amputated ear. There is venous congestion, and leeches are applied. This patient is at risk for infection by which of the following organisms?
A) Actinobacillus lignieresii
B) Aeromonas hydrophila
C) Eikenella corrodens
D) Pasteurella canis
The correct response is Option B.
Aeromonas hydrophila is an organism present in the leech species Hirudo medicinalis gastrointestinal tract that can lead to an infection if used medicinally. In this patient with venous congestion and application of leeches, antibiotic prophylaxis is recommended with fluoroquinolones, tetracycline, or trimethoprim-sulfamethoxazole.
Actinobacillus lignieresii is seen in horse bites, Pasteurella canis in dog bites, and Eikenella corrodens in human bites.
In a recent review of ear reattachment methods, a variety of approaches have been used including microsurgical reattachment, burying of the part in a subcutaneous pocket, periauricular tissue flaps for coverage of the part, and direct reattachment as a composite graft. Microsurgical replantation is associated with the best aesthetic outcome even if venous anastomosis is not possible and leeching is necessary.
2014
A 35-year-old woman with type 2 diabetes mellitus is evaluated in the emergency department because of severe pain and drainage from the right buttock 36 hours after undergoing bilateral buttock augmentation with autologous fat harvested from the thighs. Temperature is 102.0°F (38.9°C), heart rate is 105 bpm, respiratory rate is 16/min, and blood pressure is 90/60 mmHg. Physical examination of the right buttock shows brawny erythema and drainage of turbid fluid from an injection site. The patient has marked tenderness of the buttock, and the abdomen is nontender. White blood cell count is 18.5 × 109/L and serum creatinine concentration is 1.5 mg/dL. After resuscitation, which of the following is the most appropriate next step in management?
A) CT scan of the abdomen and pelvis
B) Inpatient intravenous antibiotic therapy
C) Outpatient oral antibiotic therapy
D) Surgical exploration of the wound
E) Ultrasonography of the buttock
The correct response is Option D.
The most appropriate next step in management is to surgically explore the wound in the operating room. The clinical picture is of a severe, rapidly progressing infection, possibly necrotizing fasciitis. A high index of suspicion and early treatment are vital for successful outcomes. Necrotizing fasciitis is a rare and rapidly progressive infection of the deeper layers of skin and subcutaneous tissues, easily spreading across the superficial fascial plane, with subsequent death of the overlying skin and severe systemic toxicity. Liposuction is the most frequently associated cosmetic surgery with this infection. Signs and symptoms are insidious, nonspecific, or virtually unnoticeable early in the course of the disease. Later, erythema, prominent edema, and induration appear, accompanied by intense or intolerable pain. The clinical picture evolves into systemic toxicity and eventually multiple organ failure. Risk factors for necrotizing fasciitis include diabetes mellitus, immunosuppression, age older than 50 years, malnutrition, and peripheral vascular disease.
There are two forms of the disease: one caused by Streptococcus pyogenes, and the other by mixed infections caused by a variety of microbes, including Escherichia coli, Proteus, Serratia, and Staphylococcus aureus. The progressive necrosis of the tissues typically involves the superficial fascia and the subcutaneous layer. The extent of the gangrene at the fascial layer is typically more severe and greater than at the skin level. This insidious infection is virtually unnoticeable and nonspecific in the first 24 to 48 hours; however, in the following days, an extensive, hardened area appears, which is often dark colored in the center. Intense pain and skin necrosis follow at the level of the infection. Metabolic changes occur, ending with respiratory distress, oliguria, acidosis, increased creatine kinase activity, increased troponin concentrations, and toxic syndrome. Diagnosis and treatment consists of surgical exploration and debridement that reveal necrotic, edematous subcutaneous fat. Bacteriologic analysis of exudate, cultures, and histologic evaluation complete the diagnosis.
Early diagnosis is imperative to avoid a fatal outcome. Because necrotizing fasciitis is a progressive, rapid infection, a staged “second-look” operation and, if necessary, additional debridement should be performed. The mortality rates are high and range from 20 to 70%, but decrease to 4.2% after immediate surgical intervention.
Though antibiotic therapy is an integral part of the treatment, surgical exploration is key. CT scans and ultrasonography will not change the treatment plan and are therefore not the appropriate next step in management.
2014
An otherwise healthy 35-year-old man comes to the emergency department because of a 2-day history of swelling and pain in the index and long fingers of the right hand. He reports pain when he attempts to flex these fingers or bring them together. Physical examination shows no pain with passive extension of the fingers or during axial loading. There is pain with passive adduction of the fingers. A photograph is shown. Which of the following is the most appropriate management?
A) Arthrotomy of the metacarpophalangeal joint of the long finger
B) Division of ulnar-sided Cleland ligament of the index finger
C) Dorsal and volar incisions in the proximal second web space
D) Drainage of the mid-palmar space
E) Release of the A1 pulley of the index and long fingers

The correct response is Option C.
The patient described has a web space (collar-button) abscess. Pus resides dorsal to and volar to the natatory fibers of the palmar fascia with a small connection between the two spaces passing through the natatory fibers. It is drained through proximal dorsal and volar incisions in the web space. One should not incise through the apex of the web space, as this may lead to a web space contracture.
Incisions are allowed to heal by secondary intention.
Cleland ligament is a separate portion of the palmar fascia located within the finger dorsal to the neurovascular bundle. It is distal to the purulence in a web space abscess. Absence of pain with axial loading of the digits makes a joint space infection unlikely, so drainage of the metacarpophalangeal joint is unnecessary. Some approaches to drainage of flexor tenosynovitis involve release of the proximal sheath through the A1 pulley; the appearance in the photo (lack of fusiform swelling), and absence of pain with passive extension of the fingers, make flexor tenosynovitis unlikely in this patient. Infection of the mid-palmar space would produce more proximal pain and swelling in the palm, which is not present in this patient.
2014





