Spine Flashcards
(367 cards)
Safe zone for occipital screw placement
Triangular region created by connecting 2 dots 2cm lateral to the external occipital protuberance, and a point 2 cm inferior to it
Point B on the pictures

Slip angle greater than what degree is associated with greater risk of progression?
>50 degrees

6 things to do if a neuro alert during scoliosis surgery
- check equipment
- check blood pressure >90mmHg
- check Hgb
- reverse or lessen correction
- wake up test
- remove implants if spine stable

Risks of postoperative spinal infection
Longer OR time
Immunocompromised state
Increased blood loss (decreases circulating Abx)
Poor nutritional status
Obesity (BMI >35kg/m^2)
Use of instrumentation or OR microscope
Prior spinal surgery or local radiation
Longer constructs or more extensive procedures
Tobacco or alcohol use
Multiple trauma
Anklylosing spondylitis trauma
What must you do?
CT scan of spine
Often skip fractures
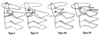
Fieldig Classification of AARD
Type I:
Unilateral facet subluxation with intact transverse ligament
Type II:
Unilateral facet subluxation with 3-5mm of anterior displacement (injured TL)
Type III:
Bilateral anterior facet displacement of >5mm
High risk of neuro compromise
Type IV:
Posterior displacement of Atlas (C1)
Safe zone for halo application (anterior pins)?
Lateral 1/3 of eyebrow, below the equator (site D in figure)
Avoids supraorbital and supratrochlear nerves

In facet dislocation, what must you do after successful reduction and why?
MRI - to look for disc herniation
What age does the secondary ossification center of the dens fuse with the rest of C2?
~12 years
Normal range of kyphosis in mid-thorcic spine (T5-12)
20-50 degrees
Power’s Ratio
Basion to posterior arch/Opisthion to anterior arch
Normal is 1
Abnormal: occipito-atlantal instability
Three types of Diastematomyelia?
- boney
- fibrous
- cartilaginous
Why do you have to use a paediatric spinal board for paediatrics? What age do you have to use it until?
To compensate for large head
Paediatric boards have an occipital cutout to compensate for this
Use until 8 years
Name 6 surgical options for degenerative spondy:
Laminoplasty
Laminectomy no fusion
Laminectomy UNinstrumented fusion
Laminectomy + instrumented fusion
(all of the above ± PLIF/ALIF/TLIF)
Dynamic stabilization (see pic)
Lumbar interspinous spacers (prevents extension)

Treatment algorithm for AARD
Acute
- Soft collar, anti-inflammatories, exercise program
Acute >1 week
- Head halter traction and bracing
Subluxation > 1month
- halo traction and bracing
Subluation > 3 months, late diagnosis or neuro deficits
- Posterior C1-2 fusion
If a patient presents with a cervical rotational deformity what injury should you think of?
Unilateral facet dislocation
Disc herniations at the following levels with affect which nerve root?
- C2-C3
- C7-T1
- T4-T5
- L2-L3
- L5-S1
1 - C3
2 - C8
3 - T4
4 - L3
5 - S1
Interpret:
a) ADI < 3 mm
b) ADI between 3 and 5 mm
c) ADI > 5 mm
a) Normal
b) Transverse Ligament Rupture
c) Transverse Ligament and Alar Ligaments Ruptured
Most common locations for pseudoarthrosis in adult spinal deformity?
L5-S1
Thoracolumbar junction
(so any junctional area)
Why is discography not so good?
It causes accelerated disc degeneration and loss of height.
What are the components of TLICS and what score means surgery?
- Morphology
- Neurologic injury
- Status of PLC
5 or more get OR
What type of vertebral malformation is most likely to cause a progressive congenital scoliosis?
Unsegmented bar with a contralateral hemivertebrae
Tx. is PSIF with resection of vertebrea
Components of PLC?
Supraspinous ligament
Interspinous ligament
Facet capsule
Ligamentum flavum
Complications of vertebroplasty/kyphoplasty
Cement extravasation
Cement Embolism
new fracture
neurologic compromise