Thoracolumbar trauma Flashcards
(35 cards)
What are osteoportic vertebral compression fractures?
- A fragilility fracture of the spine
What is the epidemiology of osteoportic vertebral compression fx?
- vertebral compression fx most common fragility fx
- 700,000 VCF per yr in US
- 70,000 hospitalisation
- 15 billion in annual costs in us
- affects 25% pt over 70years
- afects 50% over 80 years
What are the risk factors of vertebral compressono fx?
- hx of 2 VCF is the strongest predictor of future vertebral fx in post menopausal women
What is the pathoanatomy of vertebral compression fx?
- Osteoporosis
- bone normal quality but decrease quantity
- cortices are thinned
- cancellous bone has decreased trabecular continuty
- WHO osteoporosis T score -2.5 SD below normal
- BMD peaks at 25-30
- decreases with age
- correlates well w bone strength
- gd predictor of fragility fx
What are the associated conditions of osteoportic vertebral compression fx?
- Compromised pulmonary function
- inceaed kyphosis can effect pulmonary function
- each VCF leads to 9% reduction in FV
What is the prognosis of osteoportic vertebral compression fx?
- with VCF mortality increases significantly - even greater than hip fractures at 2 years
What are the signs and symptoms of osteoportic vertebral compression fx?
Symptoms
- Pain
- 25% of VCR painful enough pt seek medical advice
- pain usually localised around area of Fx
- may wrap around rib cage
Signs
- Focal tenderness
- local kyphosis
- spinal cord injury- v rare
- nerve root deficites
- may lead to foraminal stenosis
what imaging is useful for osteoportic vertebral compression fx?
- xrays
- entire spine
- concomitant spine fx 20%
- loss of anterior, middle , post vertebral height by 20% or at least 4mm
- Ct/MRI
- not normally necessary
- labs
- crp/esr- rule out infection
- urine/serum protein electrophoresis - rule out multiple myeloma
- FBC, Ca Po43-

What is the ddx of a osteoportic vertebral compression fx?
-
Metastatic cancer of spine
- must be considered and ruled out
- suspicious if
- fx above T5
- atypical radiological findings
- failute to thrive/consittutional symptoms
- younger pt with no hx of fall
What is the tx of osteoportic vertebral compression fx?
Non operative
-
Observation, bracing, medical mx
- majority tx this way
- gradual return to activity
- Bisphosphonates
- prevent fragility fx risk
- some pt benefit - extension orthosis
Operation
-
Vertebroplasty
- no recommended
- rct no benefits of vertebroplasty
- higher rate of cement extravasation assoc complx than kyphoplasty
-
Kyphoplasty
- if pt still has pain 6 wks post fx
- cavity created by expansion balloon adn therfore cement can be injected less pressure
- pain relief by elimination of micromotion
-
Surgical decompression and stabilisation
- v rare only if progressive neurology, PLL injury and unstable spine
What is the difference between kyphoplasty vs vertebroplasty?
- performed under flouroscopic guidance
- percutaneous transpedicular approach used for cannula
vertebroplasty
- PMMA injected directly into cancellous bone without cavity creation
- requires greater pressure and therefore risk of extravasation into spinal canal is greater
kyphoplasty
- cavity created with expansion device (e.g., balloon) prior to PMMA injection
- may be possible to obtain partial reduction of fracture with ballon expansion
What are the complx of vertebral compression fx?
-
Neurological injury
- by extravasation of PMMA during vertbroplasty or kyphoplasty
- NB notice defects in post cortex of vertebral body
What is a thoracolumbar burst fx?
Vertebral fx with compromise of anterior and middle column
What is the mechanism of injury to obtain a thoracolumbar fx?
- axial load with flexion
- canal can be compromised by retropulsion of fx
- maximal retropulsion at time of injury
- reabsorption of retropulsed fx does occur over time, rarely caused neurological compromise
What was Denis 3 column theory?
aim at determining stability of fx
anterior column
- ant 2/3 vertebra and annulus
- ALL
middle column
- post 1/3 of vertebra and annulus
- PLL
posterior column
- pedicels
- facets
- ligamentum flavum
- spinal processes
- post ligament complex- infraspinous, supraspinous, lig falvum, facet capsule- meant to be critical predictor of stability of fx

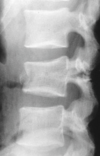
What is seen on imaging?
- Xray
- intraspinal distance increases
- pedicles widening- AP
- kyphosis
- Retropulsion
- >50% loss in height
What classificaiton system is useful to aid tx of thoracolumbar fx?
- ThoracoLumbar Injury Classification Severity Score= TLICSS
- Varacco et al modified
- Modification of the Thoracolumbar Injury Severity Scale (TLISS) based on observations from the TLISS validation study
- Modifications to improve validity and reliability
- Fracture mechanism category changed to fracture morphology
- Subcategory summation discarded (previously multiple injuries within a category were summed to a total point value.
- Lateral compression category discarded (weak reliability)

Describe the TLICSS ?
- Uses point system to guide management and is based on 3 categories: fracture morphology, neurologic status, and integrity of the posterior ligamentous complex.
f_racture morphology_
- Compression fx 1
- Burst Fx 2
- Translational/ Rotational 3
- Distraction 4
Neurology
- Intact 0
- Nerve root 2
- Complete SPI 2
- Incomplete SPI 3
- Cauda Equina 3
Posterior ligamentous complex intact
- Intact 0
- Injury suspected/indeterminate 2
- Injured 3
Summation of points
- 3 or less = non operative
- 4 non vs surgery
-
5 or more =surgery
*
What tx available for thoracolumbar fx?
Non operative
- to protect neural elements
- prevent further collapse
- restore biomechanics
- Juwett brace- 3 point fixation: pelvis, chest and lumbar spine
Surgery
- Anterior decompression and stabilization
- for neurology with ant compression
- no evidence for early surgery
- invoves corpectomy, cage
- Posterior decompression and instrumental fusion
- use to instrument 3 levels above and 2 below but now with pedicles screws one above is fine

Complications of thoracolumbar fx?
- Pain
-
Progressive Kyphosis
- common with unrecognised injury to PLL
-
Flat back
- leads to pain
What is a chance fx?
- A flexion distraction injury- seatbelt injury
- maybe bony injury
- may be ligamentous injury
- more difficult to heal
- middle and posterior columns fail under tension
- anterior column fails under compression
What are chance fx associated with?
- High rate of gastrointestinal injuries 50%
What is seen of imaging for chance fx?
- Xrays
- lat and ap- see below
- MRI
- important to evaluate injury to posterior elements
- CT
- important to evaluate degree of bony injury/retropulsion of post wall into canal

What is the tx of chance fx?
non operative
- Immobilisation in cast or TLSO in extension
- neuro intact pt
- stable fx with intact post elements
- Bony chance fx
- must follow up for non union/kyphotic deformities
Operative
-
Surgical decompression and stabilisation
- unstable fx with injury post ligaments
- anterior decompression & stabilisation
- with vertebrectomy & strut grafting+ instrumentation
- posterior decompression, stablisation and compression





