Thyroid Flashcards
(19 cards)
Describe and understand the Anatomy and vasculature of the thyroid glands
Anatomy:
Sits below the thyroid cartilage (Adam’s apple) @C5-T1
Anterior to the 2nd-4th rings of the trachea
- Contains:*
- Right and left lobes of the thyroid gland
- Isthmus of the thyroid gland
Vasculature:
Three main arteries:
- Superior thyroid artery
Superior and anterior portions
-
Inferior thyroid artery
* postero-inferior* - Thyroid Ima artery
Anterior surface and istmus
Three main veins:
- Superior thyroid vein
2) Middle thyroid vein
3) Inferior thyroid vein

Describe the histology of the thyroid gland
Follicular cells are arranged arounda lumen filled colloid.
They are cuboidal

What are the steps of thyroid hormone (TH) synthesis?
- The cuboidal follicular cells synthesize thyroglobulin, which is released into the colloid.
- Production requires iodide. A sodium/iodide symporter on the basal membrane of follicular cells traps and pumps in iodide from the plasma
- A thyroperoxidase enzyme on the apical plasmalemma oxidizes
the iodide to iodine, iodinates tyrosyl residues in the thyroglobulin, and couples tyrosyl residues to produce the thyroid hormones T4 (thyroxine) and T3 (tri-iodothyronine) still bound in the thyroglobulin and, hence, inactive - TSH stimulates endocytosis of colloid and its digestion by lysosomes, to free T4 and T3

What is the fate of T4 in the bloodstream?
The main thyroid product (T4) is not the metabolically active hormone. Metabolism of T4 to produce active T3 occurs in many cells by Deiodinases (enzymes) that convert (T4 to T3)
The main thyroid product (T4) is not the metabolically active hormone. Metabolism of T4 to produce active T3 occurs in many cells by Deiodinases (enzymes) that convert (T4 to T3)
Type 1 Deiodinases- Cell surface of most cells (esp. liver, kidney, thyroid, brain)
Type 2 Deiodinases- Intracellular raises T3 in CNS, brown fat, placenta, skeletal and cardiac muscle
What is the mechanism of action of thyroid hormones within a cell?
Thyroid hormones are transported into cells and T3 acts on nuclear receptors (TRs) which increase transcripton
This interaction results in stimulation or inhibition of the production of many different proteins.
What are the cellular effects of thyroid hormones?
Increases sympathetic activity
They act to increase the basal metabolic rate, which increases O2 use and heat production.
Stimulate production of Na+/K+ ATPase (which uses 20–45% of all ATP)
Stimulate production of many proteins; stimulates protein degradation but when T3 is excessive, degradation > production
Potentiate B adrenoceptor effects, on glycogenolysis, gluconeogenesis; potentiate insulin effects, increasing glycogenesis and glucose usage
- Stimulate gut motility
- Stimulate bone turnover (breakdown > synthesis)
• Increase speed of muscle contraction.

Explain the main causes of Hyperthyroidism (high T3)
Causes
Graves’ disease—auto-antibody with stimulatory activity when it binds to the TSH receptor on thyroid cells
• Most common cause of hyperthyroidism
Pituitary adenoma producing TSH
Tumours of thyroid follicular cells can produce large amounts of T4 and T3
Iatrogenic—over-administration of thyroxine.
What are the effects of Hyperthyroidism (high T3)?
Effects
Increased basal metabolism rate
- weight loss (despite increased appetite)
- increased resting heart rate and ‘bounding’ pulse
- heat intolerance hot hands, sweaty palms
- increased sympathetic drive
- eye protrusion
- diarrhoea
- goitre
- nervousness, irritability, mood swings
What thyroid function tests would you use to diagnose hyperthyroidism and what would they tell you?
Serum TSH, free T4 (free T3)
T3/T4
decreased TSH – thyroid gland problem (tumour/graves)
Increased TSH – fault in or above pituitary gland
What is Goitre and what causes it?
Goitre is enlarged thyroid gland
(not an indication of thyroid gland activity)
Causes:
- iodine deficiency (low levels of T4)
induces TSH secretion
- Graves disease (high levels of T4)
autoimmune disease that produces thyroid
stimulating immunoglobulin - acts on TSH receptors to mimic TSH
- Tumours (benign or cancer)
How could low T4 induce a goitre?
One way is through iodide defficiency
Insufficient iodide means not producing enough T4
low levels of T4 stimulates TSH continuously
High levels of TSH stimulates the thyroid gland to increase many biochemical processes; the cellular growth and proliferation can result in the characteristic swelling or hyperplasia of the thyroid gland, or goiter.

How could high T4 induce a goitre?
ex. In Graves’ disease, overstimulation of the thyroid glad by stimulating antibodies causes the thyroid to swell.

Name 3 treatments for hyperthyroidism.
- Drugs (inhibit production)
- Radioactive iodine (131I) (destroy gland)
- Thyroidectomy (an operation that involves the surgical removal of all or part of the thyroid gland)
Explain the causes of Hypothyroidism (low T3).
MNEMONIC: HIPIG
Hashimoto’s thyroiditis
organ-specific autoimmune disease with destruction of thyroid epithelial cells
Iatrogenic
surgical removal of thyroid, damage of thyroid by
radioactive iodine, antithyroid drugs
Pituitary hypofunction
with lack of production of TSH, non-functioning pituitary adenoma, Sheehan’s syndrome
Deficiency of iodine in diet—rare since introduction of iodinized table salt and greater distribution of seafood
Thyroid hormone resistance
a number of genetic defects in the thyroid hormone receptor reduce hormone binding. The individual is hypothyroid but will have normal levels of plasma hormone.
Explain the effects of hypothyroidism.
Effects
In the neonate—cretinism leads to gross deficits in CNS myelination and stunting of postnatal growth
In the adult: myxoedema—decreased basal metabolic rate (tiredness, lethargy, weight gain), slow mentation, hypothermia, constipation.
What thyroid function tests would you request for Hypothyroidism?
Serum TSH, free T4, free T3
reduced T4 and reduced T3
TSH – usually increased
(note: slightly raised TSH with a normal T4 is called subclinical, mild, or borderline hypothyroidism)
What are some treatments for hypothyroidism?
Replacement hormones
levothyroxine (synthetic T4)
- drug of choice for maintenance
- longer half life (once a day) and activated in body
- dose titrated up
- blood tests (~ 8 weeks: aim for normal TSH)
liothyronine (synthetic T3)
- limited use
- rapid (transient) action, spikes
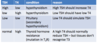
What is primary vs secondary hyper/hypothyroidism?
( primary = at the gland / secondary = outside the gland)
Primary hyperthyroidism
relates to the thyroid gland producing large amounts of hormone due to either uncontrolled growth of hormone-producing functional tissue or by way of an autoimmune process that interferes with the normal feedback control.
Primary hyperthyroidism is caused by:
Thyroid nodules
Thyroid adenoma
Graves’ disease
Thyroiditis
Secondary hyperthyroidism may be attributed to an over-stimulation of the thyroid. This may be due to increased production of TSH from the pituitary gland or TSH-secreting tumor, or more rarely from overproduction of TRH from the hypothalamus or thyrotropin-releasing hormone (TRH)-secreting tumor.
Secondary (or non-thyroidal) hyprthyroidism
Carcinoma
TSH-secreting tumors
TRH-secreting tumors
Complete this: