Type 1 Diabetes Flashcards
(27 cards)
What is the difference between Type I & Type II diabetes?
Type I diabetes is an autoimmune disorder where insulin secreting beta cells are destroyed leaving the patient unable to create their own insulin. Is usually detected earlier in life.
Type II diabetes is largely diet based and develops over time. Usually diagnosed later in life.
What are the differing rates of insulin products?
- Rapid-acting
- Short-acting
- Intermediate-acting
- Long-acting
What are the 2 administration methods for insulin?
- Conventional insulin therapy (CIT)
- Intensive insulin therapy (multiple daily injections/continuous subcutaneous insulin infusion therapy (CSII)
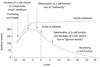
What does conventional insulin therapy (CIT) involve?
Typically 2 injections of rapid/intermediate-acing insulin before breakfast & dinner.
Provides a peak of insulin at these times and a relatively high background insulin throughout the day
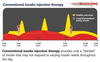
What are the benefits & limitations of conventional insulin therapy (CIT)?
Benefits:
Relitively unobtrusive.
Limitations:
Can be difficult to achieve glycaemic control
What does multiple daily injections of insulin involve?
Insulin is injected mulltiple times in one day.
Known as ‘intensive insulin therapy’.
Patients follow a basal-bolus regime.

What are the benefits & limitations of multiple daily injections/intensive insulin therapy?
Benefits:
Offers a better oppertunity than CIT to achieve glycaemic control
Limitations:
More injections that CIT which may be more difficult and more undesirable.
What does continous subcutaneous insulin therapy (CSII) (or insulin pump therapy) involve?
Consists of a small device which is attached to the patient via a cannula. Insulin is stored inside the device and is rapid-acting.
What are the benefits & limitations of continous subcutaneous insulin therapy (CSII) (or insulin pump therapy)?
Benefits:
Reduction in insulin requirements by up to 26% (Pickup, 2017)
Improvements in HbA1c (Pickup, 2008)
Reductions in severe hypoglyceamia (Pickup, 2008)
Improvements in the dawn phenomenon (Cummins, 2010)
Limitations:
Practical difficulties carrying the device (hard to wear certain clothing)
Playing sports difficult
Cannula must be replaced every 2-3 days
Still required to test blood glucose levels multiple times a day
Still required to carry insulin pen (back up)
Rapid acting insulin can deplete very fast
More expensive than MDIs

What 3 factors/aetiologies are said to play a role in the development of T1D?
Immunological factors
Environmental factors
Genetic factors
What is the name for the family of genes associated with determining risk for T1D? What alleles from this family were specifically shown to infer risk?
Human Leukocyte Antigens (HLA).
Alleles such as DR3 and DR4 were shown to infer risk
Other than the HLA-DR3 and DR4 alleles, what other genetic marker is associated with T1D? Which chromosome does this marker reside? What does this marker implicate?
IDDM2 locus which resides on chromosome 11. Implicated in insulin regulation
*Only confers approx. 10% of T1D susceptibility and highly variable between ethnicities. Is of primary importance AFTER HLA region
In addition to the IDDM2 locus on chromosome 11 associated with T1D, what other loci have been implicated in T1D?
IDDM3-IDDM18
*be aware some are only suspected and are not yet fully supported with evidence

There are a number of non-HLA and non-insulin regulating genes associated with T1D risk. What is an example of this and on what chromosome is it located? How does this gene implicate T1D?
PTPN22 (protein tyrosine phosphatase nonreceptor type 22) found on chromosome 1p13.
Implicated in the prevention of T-cell activation by way of reducing T-cell receptor signalling
If an individual has a gene associated with T1D, are they guaranteed to develop the disease?
No.
E.g. rates of T1D are continually increaseing however the high-risk HLA genotype remain static. This is in agreement with the hypothesis that environmental factors may be driving the increase in incident rates.
What are the environmental factors proposed by both the DiaMond study and EURODIAB study? What type are thought to be the most likely candidate?
That geographical differences of disease incidence could indicate a viral trigger
Enteroviruses - enterovirus mediated damage to pancreatic beta cells have been clarified
What did the DAISY study and TEDDY study find about T1D?
There was no association found with viral infections and the onset of T1D
Aside from viral infections, what other potential environmental factors could be associated with T1D?
- Birth Process (cesarean)
- Breastfeeding
- Childhood obesity
- Gluten sensitivity
- High CHO intake
Is the onset of T1D linear?
No. it happens in distinct stages measured in month/years.

What are the symptoms diplayed by someone who may be suffering from T1D?
- Tiredness/fatigue
- Frequent urination
- Excess hunger and thirst
- Wounds that won’t heal
- Numb/Tingling hands and feet
- Weightloss
What are some current and future developments in T1D?
Continuous glucose monitoring (CGM) devices
What are some differences between T1D and T2D?
T1D:
- Insulin deficiency
- Occurs primarily in children and young adults
- Less common than T2D
T2D:
- Inadequate response to insulin
- Typically onsets during adulthood
- More common than T1D (90% of cases)
*both manifest as increased glucose levels in the blood (hyperglycaemia)

What is T2D?
A disease characterised by insulin resistance and a gradual destruction of pancreatic beta-cells leading to an increase in blood glucose levels or hypergylcaemia.
Occurs in older, overweight or obese adults
Can be hereditary (CAPN10 and TCF7L2 genes)
What is insulin resistance (IR) in T2D?
Where the body produces insulin but is unable to use it effectively.