Week 1 & 2 Intensive Flashcards
What are the effects/ side effects of Barbiturates?
* CNS: depression, GABA receptors (inhibitory neurotransmitters bind), NO analgesia
* CV: increase in HR, decrease in arterial BP (decrease peripheral resistance, decrease SV, myocardial contractility), increased sensitivity of myocardium to cirulating catecholamine (arrhythmias common at induction)
* Resp: post-induction apnoea common especially following opioid premed, decreased ventilatory rate and tidal volume
How can you monitor the time, temperature and air removal of the steam sterilisers? Which class do you want?
* Chemical indicators
* Want class 6: it covers all variables with greater specificity/ reliability.. where class 1 changes colour to indicate it has been exposed to heat only
What are the disadvantages of inhalation anaesthetics?
* Requires expensive equipment (anaesthetic machine and vaporizer, breathing circuit and scavenger system)
* Must have an intimate understanding and know how to trouble shoot this equipment
* Must test this equipment before each case, and perform regular maintenance
* Significant dose-dependent depression of CV and respiratory function
What is different about monitoring small ruminants under GA?
* Rotation of the eye is not a useful indicator of anaesthetic depth
* HR should be within normal limits, 80-120 beats
* RR should be between 20 and 40 breaths/min
What would you tell the owner?

50% chance the dog will live for longer than 21 months with treatment. Less than 20% chance it will be alive at 2 years.
What are inhalation anaesthetics? What is vapour pressure? What is the vapour pressure for Isoflurane? What is the vapour pressure for Sevoflurane?
* Inhalation anaesthetics are volatile liquids that evaporate or vaporize at room temperature and pressure
* The vapour pressure of an inhalation anaesthetic is a measure of its ability to evaporate at a given temperature (20C) and pressure (1 atm= 760 mmHg)
* Isoflurane: 240 mmHg @ 20C and 760 mmHg
* Sevoflurane: 160 mmHg @ 20C and 760 mmHg
What side must the sheep be on for an endotracheal intubation?
Left side lateral recumbency- head going down
What is the problem with partial agonists and agonist-antagonists? How are pure agonists better?
They are unreliable, they are only “sometimes” potent analgesics
* They are reliable, best for severe pain, can be topped up
Why should you never administer anticholinergics with alpha 2 adrenoceptor agonists to offset the bradycardia?
Severe hypertension can result
When might you use Fentanyl and Alfentanil? What are the dangers?
* Fentanyl is 100 x more potent than morphine and alfentanil is 50 x more potent
* short acting agents- mainly used intra-op as bolus or infusion
* useful for animals who emerge in severe pain
* bradycardia and resp depression common!
What are repercussions of pain?
* Sleep disorders (anxiety)
* Aggressivity
* Neuroendocrine modifications- resp function, CO, decrease gastric and intestinal motility, electrolytes in balance
* Hypothalamo-hypophyso-surrenalian axe
- Glucocorticoids= hyperglycemia, catabolism of protein, depression immune system
Induction and maintenance dose of sevoflurane?
Speed of induction, recovery and depth during maintenance?
Induction: 5%
Maintenance: 2-3%
* Faster induction and recovery and changes in depth during maintenance than with halothane and isoflurane
What are the physiological effecst of opioids?
* CNS depression (or excitement in horses and cats)
* CVS: minimal effects, possible sinus bradycardia (vagal centre)
* Respiratory system (depression, drug and dose-dependent)
* histamine release (pethidine and morphine)
* GIT depression
* Release of ADH (urine retention)
* Hypothermia (sometimes hyperthermia in cats, horses, swine)
* Emesis (CTZ)
* Pupillary diameter (miosis in dogs; midriasis in cats)
What is Preferred Body Temperature (PBT)?
* the temperature at which metabolism is optimal
What would a vaginoscopy show in pro-oestrus? Oestrus? Dioestrus?
* pro-oestrus: pink, swollen, rounded folds, moist
* oestrus: pale-pink, shrunken/angular (crenulated), dry
* dioestrus: hyperaemic areas, rounded folds
What is the rate at which equilibrium is reach determined by?
* anaesthetic concentration gradient
* solubility in blood and tissues
* changes in alveolar ventilation
* changes in alveolar blood flow
* changes in matching between alveolar ventilation and blood flow
Drugs for a seizure in a dog?
* Diazepam
* Midazolam
* Levetiracetum
What does chemosensitivity (sensitivity of the tumours are to chemo drugs) depend on?
* Drug uptake into cell
* Interaction with cellular target
* Generation of lethal damage to cell
* Repair and response to that damage
What is a flail chest?
Ribs are broken, tries to breathe in = ribs collapse
What does vaginal cytology reflect? What is it not useful for?
* Vaginal cytology reflects endogenous oestrogen levels
* Excellent to determine dioestrus (D1)
* Good to determine proestrus or anoestrus
* NOT useful to determine ovulation or ideal time of breeding
MCV? MCH? MCHC? RDW?
MCV (PCV/RCC)- Mean corpuscular (red cell) volume– measures the volume of all the red cells going through and avgs it
MCH (Hb/RCC)- mean corpuscular haemoglobin (how much Hb does each red cell have)
MCHC (Hb/(RCC x MCV))= mean corpuscular hemoglobin concentration (** MORE SPECIFIC MEASURE)
RDW- red cell distribution width (measure of anisocytosis)
NRBC- nucleated red blood cells
Primary vs. delayed haemorrhage
* primary- inevitable but this can be reduced by good surgical technique and preemptive haemostasis
* delayed haemorrhage can be due to inadequate primary haemostasis (often masked anaesthesia induced hypotension) or failure of haemostasis (e.g. slipped ligature or necrosis of ligated/ coagulated vessels)
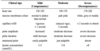
What are the commonly used classes and drugs in those classes in vet medicine?
* Phenothiazine: Acepromazine
* Alpha-2 adrenoceptor agonists: Xylazine, (dex)medetomidine, romifidine, detomidine
* Benzodiazepine: Diazepam, midazolam