Week 2 Flashcards
(24 cards)
What is Seidel’s Test?
After adding fluoroscein to an injured eye, the fluid can be visualised becoming more and more diluted as it flows out at the site of injury
Lipid-soluble drugs penetrate the ____
Water-soluble drugs penetrate the ____
Name a drug used in ophthalmology that has both hydrophilic and lipophilic properties and therefore can penetrate the cornea easily
Lipid soluble penetrate the epithelium (which is lipophilic and hydrophobic)
Water soluble penetrate the stroma (which is lipophobic and hydrophilic)
Chloramphenicol has both hydrophilic and lipophilic properties
What anti-inflammatory agents are used in ophthalmology?
Steroids
NSAIDs
Anti-histamines
Mast cell stabilisers
What are some of the side effects of steroids, both locally (in the eye) and systemically?
Local
- Cataracts
- Glaucoma
- Exacerbation of viral infection (e.g. in Herpes zoster)
Systemic
- Gastric ulcers
- Immunosuppression
- Osteoporosis
- Weight gain
- Diabetes
- loads more…
Order these topical steroids from weakest to strongest…
- Betamethasone
- FML
- Dexamethasone/Prednisolone
Predsol
FML
Predsol
Betamethasone
Dexamethasone/Prednisolone
How would a patient with glaucoma present in terms of visual defect?
What treatments can be given?
Patients with glaucoma initially lose peripheral vision, then in the later stages central vision is affected
Treatments aim to “turn off the tap or open the drain” i.e. relieve pressure
Prostanoids e.g. Latanoprost
Beta-blockers e.g. timolol
Carbonic Anhydrase Inhibitors e.g. Dorzolamide (topical) or Acetazolamide (systemic)
Alpha2 adrenergic agonists e.g. Brimonidine
Parasympathomimetic e.g. pilocarpine
What is one of the main issues with regards to medication for glaucoma? What is a potential solution?
Compliance is the issue!
Can be solved with intravitreal injection - delivers effective conc. of drug to site but many drugs are toxic to the retina
Can also be done to treat Endophthalmitis and deliver steroids/anti-VEGF
What is endophthalmitis?
Inflammation of the interior eye, usually due to bacterial infection
Possible complication of surgeries to the eye, including procedures for glaucoma. Potentially sight-threatening and antibiotics need to be given ASAP
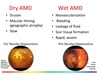
What is the difference between wet and dry age-related macular degeneration?
Dry - most common form, slow and gradual progression of blurry vision, painless. “Drusen” (yellow spots) may be seen on fundoscopy
Wet - sudden onset of vision loss, caused by the development of new blood vessels. “Scotoma” (dark spots) may be seen on fundoscopy
What are the 3 C’s that have to be mentioned when inspecting the back of the eye on fundoscopy?
Cup size (disc to cup ratio is 0.2-0.6)
Colour
Contour
List some causes of sudden onset visual loss
Vascular causes
- occlusion of retinal circulation/optic head circulation
- abnormal blood vessels e.g. diabetes retinopathy, wet ARMD), retinal tear
Vitreous haemorrhage
Closed-angle glaucoma
What arteries supply the eye?
Central retinal artery - supplies the inner 2/3rds of the retina (outer 1/3rd is supplied by the choroid)
Posterior ciliary arteries - mainly supply the optic head
What are some of the signs and symptoms of Central Retinal Artery Occlusion (CRAO)
What causes CRAO?
Signs
- RAPD (relative afferent pupil defect)
- Pale, oedematous retina, thread-like vessels
Symptoms
- Sudden visual loss
- Profound i.e. can’t count fingers
- Painless
CRAO is a type of stroke, most commonly caused by carotid artery disease but also less commonly caused by emboli from the heart

CRAO - treatment
If presenting within 24 hours - try ocular massage in an attempt to convert from CRAO to BRAO
Vascular management - establish the source of the embolus via carotid doppler and assess and manage risk factors
What is amaurosis fugax?
(HINT - this translates to “fleeting darkness”)
How is it managed?
Transient CRAO - temporary, painless visual loss
Described as being like “a curtain coming down” over the vision
Lasts ~5 mins with full recovery
Management - urgent referral to Stroke Clinic and give Aspirin
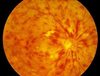
What are some of the signs and symptoms of Central Retinal Vein Occlusion (CRVO)?
How would it appear on fundoscopy?
Signs
- Retinal haemorrhages
- Dilated, tortuous veins
- Disc and macular swelling
Symptoms
- Sudden visual loss
- Moderate to severe, anywhere between 6/9 to perception of light
Arterial occlusions in the eye are due to stasis/emboli
Venous occlusions in the eye are due to stasis/emboli
Arterial = emboli
Venous = stasis
What is occlusion of the posterior ciliary arteries also known as?
What are the two types of this occlusion, and what commonly causes each?
How does this condition present on fundoscopy?
Also known as Ischaemic Optic Neuropathy
Types
- Arteritic (50%), caused by inflammation (e.g. GCA)
- Non-arteritic (50%), caused by atherosclerosis
On fundoscopy a pale, swollen disc is seen

What are some of the important symptoms to be aware of for Giant Cell Arteritis?
Headache
Jaw claudication
Scalp tenderness
Amaurosis fugax
Malaise
Very high ESR, PV and CRP
Tender/enlarged scalp arteries
What are some of the signs and symptoms of Vitreous haemorrhage?
How might it present on fundoscopy?
Symptoms
- Loss of vision
- Floaters
Signs
- Loss of red reflex
- May see haemorrhage of fundoscopy

If a patient presented with sudden onset of flashes and floaters and a painless loss of vision, what might be the cause?
Which group more commonly gets this condition?
Could be retinal detachment
More common in Myopes (short-sighted individuals)
How is closed-angle glaucoma brought about?
Aqueous humour encounters increased resistance through the iris/lens channel
Increased pressure = iris bows forward and obstructs the trabecular meshwork

How will a patient with closed-angle glaucoma present, and how do they need to be managed?
Presentation
- painful, red eye
- visual loss
- headache
- nausea and vomiting
Management
- requires urgent drops/oral medication to lower IOP and prevent patient from going blind
- follow up with laser iridotomy to unblock trabecular meshwork
List some of the causes of gradual visual loss
Cataracts
Dry ARMD
Refractive error
Glaucoma (open-angle)
Diabetic retinopathy


