Week 2 Flashcards
(122 cards)
How long can sperm survive in the female genital tract?
How long do ovum survive in the female genital tract?
5 days
17-24 hours
How does cervical position vary during fertility?
More fertile - cervix is high in the vagina, soft and open
Less fertile - cervix is low in vagina, firm and closed
In a ‘regular’ 28 day menstrual cycle, which days are considered to be the most fertile?
8-18
What are the 3 criteria for lactational amenorrhoea?
How effective is this as a contraceptive?
1) exclusively breast feeding
2) less than 6 months post natal
3) amenorrhoeic
98% effective (woman will still ovulate after delivery, hence why not 100%)
What is the mode of action of the combined oral contraceptive pill (COCP)?
Primarily inhibits ovulation through negative feedback on pituitary via oestrogen and progestogen
Also has an effect on cervical mucus and the endometrium
What kind of contraception is desogestrel?
How does it work?
Newer progesterone-only pill (POP)
Inhibits ovulation (NB - older POPs don’t inhibit ovulation!)
Also has effects on cervical mucus, fallopian tube transport and endometrial thickness
How long does the contraceptive implant last for?
What is its mechanism of action and how effective is it?
Up to 3 years
Main mode of action is inhibition of ovulation (and again, has effects on endometrium and cervical mucus)
Failure rate is 0.05% - very effective as it doesn’t rely on patient compliance
How long does the depo injection last for?
What is its mechanism of action and how effective is it?
Depo injection is repeated every 13 weeks, but lasts 14 weeks
Primarily inhibits ovulation
Failure rate is 0.2%
What are the 3 doses of IntraUterine System (IUS) currently available?
What is their mechanism of action and how effective are they?
Mirena - 52mg
Kyleena - 19.5mg
Jaydess - 13.5mg
Releases a small amount of hormone daily and mainly causes contraception through affecting implantation (renders the endometrium unfavourable)
High frequency pulses of GnRH result in release of ____
Low frequency pulses of GnRH result in the release of ____
High frequency pulses = LH release
Low frequency pulses = FSH release
What is the mode of action for the intrauterine device (IUD)
How long is it licensed for and what is the failure rate?
Primary mode of action is prevention of fertilisation - causes an inflammatory response in the endometrium and is toxic to both the sperm and the egg
Licensed for 5/10 years
What is the most effective form of contraception, based on % of women experiencing pregnancy in their first year of use?
Progesterone only implant (0.05%)
Before providing contraception, what examinations are done by the clinician?
Depends on the contraceptive being given
BP and BMI are recorded (a lot of options increase weight due to affecting appetite)
Check smear status if relevant
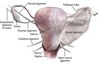
PV to check uterine size/position if required for IUD fit
What forms of contraception may be quick-started (started immediately and not waiting until next period) and which should not be?
Possible to Quick start
- Some CHCs
- POP
- Implant
- (Depo)
Avoid
- IUD (may cause miscarriage)
- Pills containing cyproterone acetate
When is emergency contraceptive required?
When contraception hasn’t been used/used correctly
Before new contraceptive method has had a chance to become effective
If more than one COC has been missed
If patch/ring has been off/out for more than 48 hours
If an implant has been fitted out with the first 5 days of cycle, and unprotected sexual intercourse has happened within the first 7 days of use
Up to 5 days after UPSI or within 5 days of predicted ovulation
What methods of emergency contraception are currently available?
Which is most effective?
Intrauterine
- copper IUD - TEN TIMES MORE EFFECTIVE than oral alternatives
Oral
- LNG-EC - up to 72 hours post UPSI (96 hours off license)
- UPA-EC - up to 120 hours post UPSI
Why can the copper IUD be used at emergency contraceptive up to 5 days post UPSI, or after 5 days after likely ovulation?
Because pregnancy doesn’t implant during the first 5 days post-fertilisation. Most happen at days 8-10, but earliest is 6
How does oral emergency contraceptive work?
LNG-EC - high dose progestogen (works before LH surge)
UPA-EC - anti-progestogen (works until after start of LH surge)
Both DELAY ovulation but neither are abortifactant and NEITHER work after ovulation

Under what circumstances should someone avoid UPA-EC?
If they are wishing to quick-start a hormonal contraceptive
They must delay their ongoing contraception for 5 days
If hormonal contraception has been used in the past 7 days
If the patient has acute severe asthma that is uncontrolled by oral steroids
Other than contraception, what are some of the other benefits of using hormonal contraception
Manage heavy menstrual bleeding
Managing painful periods
Managing irregular periods
Managing premenstrual symptoms
Endometriosis (oral contraptive helps to manage symptoms and prevent progression)
PCOS
Managing menstrual migraine
Acne, mood, hirsutism
Protection from certain cancers - endometrial, ovarian
Prevention of osteoporosis
What forms of combined hormonal contraceptive are there?
Combined oral contraceptive pill
Combined transdermal patch
Combined vaginal ring
What is the efficacy like for combined hormonal contraceptive?
How does weight affect this?
If perfect compliance - 0.3% failure rate
Typical compliance rate - 9% failure rate (people forget to take pill!)
The transdermal patch may have a possible decrease in efficacy in patients over 90kg
How should the combined oral contraceptive pill be taken?
Start in first 5 days of regular menstruation OR at any time in cycle when reasonably sure not pregnant, plus condoms for 7 days (“belt and braces”)
Take daily for 21 days followed by a 7 day break (during which there will be a period-like bleed) then start a new pack
By what mechanism might the combined hormonal contraceptive be thrombogenic?
Alteration in antithrombin III and Protein S, affecting the body’s natural coagulation defences