Week 5: Muscles Flashcards
(42 cards)
Where is the contraction signal passed between muscles? What are the two major structures that allow for signals to be passed?
The AP travels along the surface membrane and enters the actual muscle structure via the t-tubules (transverse) at the end of sarcomeres. The depolarization of the t-tubule is passed to the sarcoplasmic reticulum.

What are the structures that contain the Ca2+ necessary to depolarize the muscle cell and allow for contraction?
The terminal cisternae and sarcoplasmic reticulum contain Ca2+ that allows for depolarization

Why does K+ not re-enter cells as quickly in muscles, and what is the significance of this? What helps with repolarization?
The space between cells is limited, and forces K+ to remain in the intercellular space. This prevents muscle cells from hyperpolarizing as significantly and as quickly as a nerve cell might. Cl- channels in the membrane allow Cl- to keep the membrane about -10mV more hyperpolarized than in a typical neuron. Cl- can enter the cell to help with repolarization.
Describe excitation-contraction coupling
The triad of t-tubules, DHP/L-type Ca2+ channels & ryanodine receptors, and sarcoplasmic reticulum aid in this process. The depolarization of t-tubules couples with the release of Ca2+ from the sarcoplasmic reticulum. The DHP/L-type Ca2+ channels are activated by the depolarization, and activate the ryanodine receptors to release Ca2+ from the SR. The interaction of ryanodine/DHP is NOT mediated by Ca2+, but instead by a physical interaction (conformational change) between the two where the change causes ryanodine to open Ca2+ channels.
What muscle fibers are involved in contraction? Of the I and A bands, which one moves (shrinks) during a contraction, and which one does not change in length? What structure are all of these found within?
In skeletal muscle, actinandmyosinare both involved in the contraction of muscle cells. TheA bandis composed ofmyosin, and does not shorten, but rather pulls along the neighboringactin fiber. TheI bandis the distance between the ends of myosin fibers, and shortens as the end-to-end myosin fibers move along the actin fibers towards one another. These are all found withinsarcomeres.

What are the names for the midlines of the actin and myosin fibers in muscle?
The midline of myosin is found at the M-line. The midline of actin is found at the Z-line.

Describe the structure of troponin and tropomyosin
Troponin and tropomyosin are both found on ACTIN filaments. There are three subunits of troponin
Troponin-T is anchors the head structure to tropomyosin. Troponin-I locks tropomyosin in place, Inhibiting it from interacting with myosin. Troponin-C binds Ca2+, moving tropomyosin away and allowing actin and myosin to interact.

Describe the interaction of tropomyosin components that allow the head to move along actin filaments
Troponin C binds Ca2+ and causes tropomyosin to move out of the way of the active site on actin. Myosin heads can then bind and execute a POWER STROKE.
Describe how ATP helps drive filament contraction
When ATP is bound to the myosin heads, myosin cannot bind to actin. The Ca2+ ATPase on the myosin head cleaves ATP into ADP and Pi, allowing the head to become perpendicular to the actin filament. Ca2+ binds to the head and forces a conformational change that allows the myosin head to attach to actin. The power stroke occurs when ADP + Pi is released from the troponin head, as ATP hydrolysis has provided energy for this motion. The myosin head bends 45 degrees, pulling it along the actin filament. A new cycle begins when ATP once again binds to the head. A lack of ATP means the cycle cannot occur (as in rigor mortis–ADP remains bound and contracted, as it cannot be replaced by ATP)
Where does the ATP required for skeletal muscle contraction derive from? At the end of muscular work/contractions, how is ATP used to restore the system?
The glycolytic pathway (leads to acidosis), oxidative phosphorylation, and creatine/creatine phosphate stores. ATP is also used to move Ca2+ back into the SR.
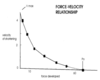
Describe the length-tension relationship
Maximum force is generated when there is maximal overlap between actin and myosin filaments (point 3 in le photo)
Little overlap or total of actin/myosin means no/few new cross-bridges are formed, so little/no tension is produced (numbers 1/5)

What is isotonic contraction? What is isometric contraction?
Isotonic (same tension) contraction occurs when the muscle maintains the same amount of tension as it shortens. Examples include walking, running, or lifting a light object. Isometric (same length) contraction occurs when the muscle does not shorten, and the tension of the muscle never exceeds that of the opposing force. HOWEVER, the individual muscle fibers will shorten. Examples include holding a weight in place above the ground or pushing against a nonmoving object (a wall).
What are the forms of isotonic contraction?
Concentric, where muscle fibers contract or shorten, and eccentric, where muscle fibers lengthen
What are the terms for the building and destruction of muscle?
Hypertrophy involves the growth of muscles by the addition of sarcomeres to a bundle, and hyperplasia involves the shrinking/deterioration of muscles by removal of sarcomeres.
Explain the concept of tetanus
Repetitive stimulation of a muscle increases its tension by summation of the signals. Contractile responses (twitches) can add two APs together, creating a graded increase in force. If a muscle fiber is stimulated twice in quick succession, it cannot relax, and the twitches merge into a sustained contraction called tetanus. Twitch summation usually results from sustained elevation of Ca2+ in the cytosol

What is a common way to regulate muscle strength?
One common method is to change the number and type of motor units involved in contraction. Multiple individual motor units can be stimulated by the same alpha motor neuron, and therefore can be stimulated simultaneously. This may allow a white and a red muscle cell type to be activated at the same time, or in other words, fast and slow twitch. This allows us to have both fine, controlled movements, as well as strong, forceful ones.
What is the innervation ratio?
It is the ration of muscle fibers to nerve fibers in a motor unit. Fitnesses of a given type of movement are functions of the innervation ratio.
What are the difference between type 1 and type 2 muscle cells?
Type 1: Slow twitch (low force)
Nerves are small, easily excitable, fairly fast. The muscles use oxidative phosphorylation pathways to generate ATP, and thus can endure stimulation for a long period of time. This is also known as “red” muscle, because capillaries infuse with these muscle cells to deliver oxygen (via myoglobin) to mitochondria there for oxidation.
Type 2: Fast twitch (high force)
Nerves are large, difficult to excite, and very fast. The muscles use glycolysis to generate ATP, and thereby create lactic acid buildup in the process. They fatigue easily, and are called “white” muscles because they do not need oxygen to undergo anaerobic glycolytic processes. Because they use the glycolytic pathway to generate ATP, these muscular processes are fat-burning!
What are some ways muscle fibers can adapt to the demands placed on them?
Enduance exercise (running) can promote oxidative capacity in red muscle fibers, allowing them to utilize oxygen more efficiently.
High-intensity resistance training (lifting) promotes hypertrophy of fast glycolytic fibers, causing them to increase diameter. Testosterone promotes protein synthesis for this increase, and weight training can convert fiber types between Type I and II. However, skeletal muscles can also atrophy when not used.
Why is smooth muscle not striated?
The type of contraction of smooth muscle differs from that of skeletal muscle. Whereas skeletal muscle contractions depend on longitudinal shortening for pulling on tendons, smooth muscle actin and myosin fibers are networked like a web to pull multidimensionally, creating muscular “waves,” and more. They help change the diameter of blood vessels, promote movement of material through hollow organs like the GI tract, and more.
What are the main differences between unitary/visceral and multiunit smooth muscle?
Visceral/unitary smooth muscle contractions are myogenic (do NOT require nerves)! A group of interconnected cells called a syncytium are connected by gap junctions, which allow for ion concentrations to shift between cells, activating contraction. These slow-wave potentials spread to the entire unit of connected cells. Examples include the GI tract, uterus, and ureters.
Multiunit smooth muscle contractions are neurogenic (DO require nerves). These exhibit properties partway between skeletal and unitary smooth muscle. They normally respond to nerve impulses, and are found in the walls of large blood vessels, airways of the lung, the bases of hair follicles, and more.

What connect the filaments in smooth muscle?
Actin filaments are connected by dark bodies scattered throughout the cytosol, and use sliding filaments of actin and myosin for contraction.
Gap junctions also connect neighboring fibers of unitary smooth muscles, allowing the AP generated in one fiber to travel to others. On the other hand, each multiunit smooth muscle cell is completely insulated and each fiber is insulated.
What are the three types of smooth muscle APs?
(1) Single spike (electrical stimulation, muscle stretch)
(2) plateau (prolonged contraction, bladder/uterus)
(3) slow waves (very long, slow, as in intestines)

What is the difference between surface elements of smooth and skeletal muscle?
Unlike skeletal muscle cells, which have t-tubules, connective SR and consistent NMJs, smooth musle has calveoli (singular: calveolus) that are depressions in the membrane that usually are studded with voltage-gated Ca2+ channels.