Week 6 Flashcards
(35 cards)
What are some pre-disposing risk factors to DVT and PE?
Contraceptive pill and hormone replacement therapy
Pregnancy
Pelvic obstruction
Trauma, trauma, immobility
Malignancy
Pulmonary hypertension
Obesity
PE - signs
Tachycardia
Tachypnoea
Cyanosis
Fever
Low BP
Crackles
Rub
Pleural effusion
CXR
- Normal prior to infarction
- Basal atelectasis and consolidation follow
Shock Lung is a type of ARDS, what causes it?
Sepsis
Diffuse infection
Severe trauma
Oxygen
Pulmonary oedema causes an obstructive/restrictive pattern of disease
Restrictive
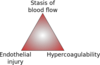
What are the three components of Virchow’s Triad?
- Factors in the vessel wall i.e. endothelial injury
- Abnormal blood flow (venous stasis)
- Hypercoaguability (cancer patients, post-MI patients)
Name one thrombolytic drug
Tenecteplase - activates tissue plasminogen (tPA)
Only for large life-threatening PEs
What is sleep apnoea? What are the risk factors?
Intermittent upper airway collapse in sleep
1-4% of the adult ppn suffer
Risk factors
- enlarged tonsils
- obesity
- hypothyroidism, acromegaly
- oropharyngeal deformities
- neurological - stroke, MS etc.
- Drugs - opiates, alcohol etc.
Depending on their size, pulmonary emboli may present in different ways. Examples of small, medium and large presentations
Small
- often clinically “silent”, subacute
- progressive breathlessnes
- pulmonary hypertension
- right heart failure
Medium
- pleuritic pain
- breathlessness
- haemoptysis
Large
- cardiovascular shock
- low BP
- central cyanosis
- sudden death
Pulmonary emboli are often subclinical - true or false
What is the source of most pulmonary emboli?
True
DVT of lower limbs is most commonly the source.
95% of PEs are thromboembolisms
What is stridor?
A predominantly inspiratory wheeze due to obstruction in the large airways
Sleep apnoea - treatment
Continuous Positive Airway Pressure (CPAP)
What cellular pathology is seen in ARDS?
Fibrinous exudate lining the alveolar walls - hyaline membranes
Cellular regeneration
Inflammation
DVT - clinical presentation and differential
Presentation
- Depending on the site, the whole leg could be affected, or just the calf
- Leg appears swollen, hot, red and tender
Differential
- Popliteal synovial rupture (Baker’s Cyst)
- Superficial thrombophlebitis
- Calf cellulitis
Warfarin and LMW Heparin are anti-coagulants with long half-lives, so may need to be reversed. How is this done?
What is the downside of the NOACs?
Reverse warfarin with vitamin K1
Reverse heparine with protamine
The NOACs have no reversal agent
Name 2 pharmacological methods of DVT prevention
Subcutaneous low dose low molecular weight heparin (Fragmin) given as a once daily injection - also start Warfarin at the same time as heparin, and continue Warfarin treatment for 3-6 months
Novel Oral Anticoagulant therapy (NOACs)
- Dabigatran - directly inhibits thrombin
- Rivaroxaban - directly inhibts factor Xa
What is pulmonary infarction?
Blockage resulting in ischaemic necrosis
Pulmonary emboli are necessary but not sufficient alone
What is the difference between a proximal and distal DVT?
Proximal
- Ileo-femoral
- most likely to embolise
- most likely to lead to chronic venous insufficiency and leg ulcers
Distal
- Popliteal
- least likely to embolise
Anaphylaxis - treatment
IV Adrenaline
IV antihistamine
IV corticosteroid
High flow O2
Nebulised bronchodilators
Suspect DVT? Investigate! What do you do?
Doppler Ultrasound (1st line)
- Non-invasive, easy
- Excludes popliteal cysts and pelvic masses
CT scan
- Visualise the ileo-femoral veins, IVC and pelvis
Causes of transudate pleural effusion (low protein)
Cardiac failure
hypoproteinaemia
Causes of exudate pleural effusion (high protein)
Pneumonia
TB
Connective tissue disease
malignancy
What conditions could be affecting the supraglottis/larynx that would result in stridor?
Laryngomalacia
- “soft larynx”, most common cause of stridor in children
- immature cartilage of the larynx collapses inwards during inhalation, causing obstruction
Supraglottic mass
Glottic lesions
Vocal cord paralysis
Think stridor? Investigate! What do you do?
Laryngoscopy
Bronchoscopy
CXR
Other imaging - CT, thyroid scan
How is cor pulmonale caused?
Feature of right sided heart disease secondary to lung disease
Specific Causes
- ARDS
- COPD
- Primary pulmonary hypertension
- Pulmonary emboli
- ILD
- CF
- Sarcoidosis



