(14.1) Pulmonary Pathology (Singh) Flashcards
(84 cards)
Describe the progression of normal fetal lung development
Embryonic (lung bud) –> Pseudoglandular –> Canalicular –> Saccular –> Alveolar

What are the clinical uses for knowing the stage of fetal lung development?
Knowing the stage can help the clinician determine the age of the fetus
What are the requirements for normal fetal lung development?
- Space in the thoracic cavity
- Ability to inhale (chest call must be able to move, and there must be enough material (amniotic fluid) present to inhale
What are the main structures you will see histologically of the trachea and main bronchi?
Cartilage
Glandular tissue
Respiratory epithelium
Smooth muscle layer
Lamina propria

Describe what you would encounter with a low-power image of lung parenchyma
Alveoli
Blood vessels
Bronchioles

Describe what you would encounter with a high-power image of lung parenchyma
Erythrocytes
Macrophages
Type 1/2 pneumocytes

What is CRUCIAL to the sucessful oxygen exchange occuring in the lungs?
A very THIN layer between the circulating erythrocytes and alveolar lumen

Describe the function of Type I pneumocytes
Facilitate gas exchange
*Support and line the alveoli

Describe the function of Type II pneumocytes
Product surfactant
Replace type 1 pneumocytes
***THEY ARE MODIFIED STEM CELLS HOW COOL IS THAT WOWOWOW

What is the function of alveolar pores?
Allow aeration but also bacteria/cells/exudate to travel between alveoli

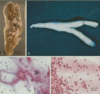
What is this pathology?

Pulmonary hypoplasia

What causes pulmonary hypoplasia?
Reduced space in the thoracic cavity (eg. diaphragmatic hernia)
Impaired ability to inhale (eg. oligohydraminos, airway malformation, chest wall motion disorders)
What is the mortality rate of pulmonary hypoplasia?
HIGH! (up to 95%)
If lung weight is <40%, immediate death occurs in neonatal period
What are foregut cysts?

Detached outpouchings of foregut
Seen along hilum and mediastinum
Can be respiratory, esophageal or gastroenteric
Often seen incidentally; complications include rupture, infection, or airway compression
Tx: Excision is curative

What is congenital pulmonary adenomatoid malformation (CPAM)?
“Arrested development” of pulmonary tissue with formation of intrapulmonary cystic masses
aka, a specific type of pulmonary tissue decides to only make a certain type of tissue for the rest of it’s life
What are pulmonary sequestrations?
Nonfunctioning lung tissue that forms as an aberrant accessory“lung bud”
*Typically found in the region of the left lower lobe
How are pulmonary sequestrations characterized?
Lack of connection to the tracheobronchial tree
Independent (systemic) arterial supply
What is this image an example of?

Intralobar pulmonary sequestration (ILS)
What are intralobar pulmonary sequestration (ILS)s susceptible to?
Lack of airway perfusion makes ILS’s susceptible to infection and absess formation

What is this an example of?

Extralobar pulmonary sequestrations (ELS)

How are extralobar pulmonary sequestrations (ELS) different from ILS?
ELS have their own PLEURA
What comes to attention sooner…
ILS or ELS?
ELS
Describe the differences between these congenital anomalies:
CPAM/CCAM
vs
Pulmonary sequestraion
CPAM/CCAM = INTRApulmonary cystic malformation w/ CONNECTION to tracheobronchial airways and pulmonary vasculature
Pulmonary sequestration = INTRA or EXTRA pulmonary lung tissue with NO CONNECTION to pulmonary vasculature or tracheobronchial tree

What is atelectasis?
Partial or complete collapse of the lung