4 - Lumbar Spine and Disorders Flashcards
(42 cards)
What are the mobile and immobile parts of the spine?
Mobile = Lumbar and Cervical
Immobile = Thoracic
What are the functions of the vertebral column?
- Protection
- Haemopoiesis
- Support
- Movement

What do the lamina and pedicle connect?
- Lamina connects transverse process to spinous
- Pedicle connects transverse to body
What are the joints like between each vertebrae?
Facet/Zygapophyseal Joints
Lined with hyaline cartilage and synovial joints
Interlocking design prevents antero-posterior displacement

What movement occurs in each region and why?
Cervical: Flexion, extension, lateral flexion, rotation
Thoracic: Only lateral flexion and rotation
Lumbar: Mainly flexion and extension some limited lateral flexion and extension from L5 as facet faces anteriorly

What other joints are there in the spine apart from facet?
Secondary Cartilaginous (Symphyses): Intervertebral discs
Fibrous: Sacro-iliac joint

What is the structure of the intervertebral discs?
- Contains water and proteoglycans too
- Discs lose height with day and age
- Slightly wedge shape posteriorly
- Avascular and aneural so all diffusion and osmosis
- Nucleus goes from central to slightly posterior as get older and has high oncotic pressure

Label this diagram with the main ligaments of the spine.


What do each of the spinal ligaments do?
Posterior Longitudinal: prevents hyperflexion from C2 to S canal. Reinforces annulus fibrosus centrally
Anterior Longitudinal: stronger than pos and prevents hyperextension. C1 to Sacrum. Blends with periosteum but loosely attached and slides over discs
Ligamentum Flavum: Yellow between laminae and adjacent vertebrae. High elastin. Stretched during flexion
Interspinous: Weak fibrous tissue between spinous processes, well developed in lumbur area, restrict hyperflexion
Supraspinous: Tips of spinous processes, lax in extension, prevent hyperflexion and mechanical stability

How do intervertebral discs mainly prolapse?
Paracentrally as posterior longitudinal ligament supporting annulus fibrosus

How should you lift heavy weights and why?
Close to you with straightback so force picking up is equal to force on back

Where does force transmission occur in the spine?
Young: 80% vertebral body, 20% facet joints
Old: Disc dehydration so 35% in facet joints, leading to osteoarthritic changes

Describe the structure of the sacral and coccygeal spine and discuss what it articulates with.
Coccyx is remnant of a tail

Where does the central canal end?
Fourth sacral at the sacral hiatus
What nerves originate from the cauda equina?
- 2nd to 5th lumbar nerves
- 5 sacral nerves
- 1 coccygeal nerve
All innervate the pelvic organs and lower limbs
What is the dural sac?
The proximal parts of the cauda equina are enclosed in tough fibrous sac that terminates at around S2

How do nerve fibres leave from the sacral vertebrae?
Posterior sacral foramina
What is the filum terminale?
Continuation of the pia mater from the conus medullaris to the first segment of the coccyx. Approx 20cm and gives longitudinal support to spinal cord

What are the curvatures of the vertebral column?

What happens to the curvature of the spine with age and in pregnancy?
- Senile Kyphosis due to loss of disc height and osteoporitic fractures
- Pregnancy leading to exaggerated lumbar lordosis to reestablish centre of gravity

Where are the weak points of the vertebral column and why are they weak?
- C1 and C2
- C7 and T2
- T12 and L1
- L5 and S1
Centre of gravity passes through these so curves needed. Junctions are from mobile to stiff so weak spots.
Allows transmission of weight into lower limbs with curves

Label the parts of this spine.

Can assess disc height and some ligaments with this

Label this MRI of the spine.
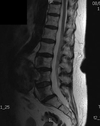
Can see ligaments and discs better

Label the ligaments of this spinal MRI


















