6 ⼀PREGNANCY II Flashcards
(270 cards)
PreEclampsia = [Gestational HTN + Proteinuria]
What are the primary components for the Mechanisms of Disease in Preeclampsia? - 4
Ab complex mediated endovascular damage –>
- Hemolytic Anemia
- Platelet aggregation from ⬆︎Thromboxane
- Vascular constriction pervasively from ⬆︎Thromboxane

PreEclampsia = [Gestational HTN + Proteinuria]
Describe timeline for Postpartum preeclampsia
PreE presents anytime between
[20WGunless 2/2 Hydatidiform Mole → PreE can present <20WG - up to 12 weeks postpartum]
_________________

PreEclampsia –> SEVERE PreEclampsia –> HELLP and at anytime, Eclampsia is possible
Nipple discharge is pathologic if it is 1 of what 3 things?
________________
How do you workup breast nipple discharge?
spontaneous | uL | persistent

The most common cause of pathologic breast nipple discharge is ⬜
[Intraductal papilloma (from lining of the breast duct ) ]

Papillomas are usually benign but may have associated carcinoma(atypical|DCIS|Invasive) within the lesion
Which contraception should be given to a patient with PCOS?
_________________
why? -2
[Progesin IUD]
_________________
androgen excess in PCOS➜ unopposed estrogen ➜ anovulation, polycystic ovaries, irregular menses, endometrial hyperplasia/CA
Progesterone Protects the Endometrium

What is 1st line tx for Dysmenorrhea in sexually active pts?
________________
What about non-sexually active pts?
Combined OCPs
_________________
NSAIDs
Combined OCPs treat dysmenorrhea by ⬇︎endometrial proliferation ➜ atrophy which –> ⬇︎prostaglandin release –> ⬇︎painful uterine contractions
Diagnostic criteria for Primary Dysmenorrhea
_________________
etx
ITSO nml pelvic exampelvic cramping during first few days of menstruation
_________________
prostaglandin release from endometrial sloughing during menses
PreEclampsia –> SEVERE PreEclampsia –> HELLP and at anytime, Eclampsia is possible
_________________
what is the treatment for HELLP? (3)
(g): B
(p): BM
(s|h|e): BMX

🧭B=[BP control: (when ≥ 140/90) = Labetalol | Hydralazine]
🧭M=[IVMG SULFATE (SEIZURE PX)]
🧭X=[X“baby out now!” = STAT IMMEDIATE DELIVERY]
What is a Hydatidiform Mole? -3
_________________
How is HM related to CA?
★ abnormal fertilization of [empty ovum (complete mole)] by either 2 sperm or [1 sperm whose genome ultimately duplicates]
Or
★ abnormal fertilization of [normal “occupied” ovum by 2 sperm ( ➜ partial mole)]
★ Moles ➜ [hypertrophic and hydropic trophoblastic villi] that secretes βhCG > 100,000
_________________
❎HM can develop into [Gestational Trophoblastic Neoplasia]
_________________
tx = [D&C + contraception] ➜ [serial βhCG until undetectable x 6 mo]

Hydatidiform Mole is a precursor to ⬜
How do you manage Hydatidiform Mole ? (5)

[Gestational Trophoblastic Neoplasia]
_________________

Tx for Trichomoniasis is ⬜(2) . What are the precautions if female patient is breastfeeding?
{[2 gm metronidazole PO x 1] + [also treat sexual partner]}
_________________
after taking, breast milk should be expressed and discarded x 24h

Give brief descriptions that differentiate Postpartum
Blues vs Depression vs Psychosis
- Blues = onsets PPD1, peaking at PPD5 and subsiding PPD14, worst w/lactation
- Depression = onset between [1 month - 12 months after birth] Traditional s/s. Previous Depression hx is RF
- Psychosis = RARE but onsets IMMEDIATELY after birth
Explain how Breastfeeding is associated with iron deficiency
_________________
thalassemia< [MIX 13]< IDA
Breastfeeding only provides sufficient iron for first 6 months of life.
[infants ≥6 months] MUST be introducted [iron-rich solid foods (pureed meats/cereals)] to prevent iron deficiency anemia
_________________
(thalassemia < [Mentzer Index 13 (MCV/RBC)]< IRON DEFICIENCY ANEMIA)
There are 3 types of female Urinary Incontinence
Describe [Stress Urinary Incontinence]
urinary leakage with INC INTRAABDOMINAL STRESS (coughing / sneezing / laughing / lifting)

There are 3 types of female Urinary Incontinence
Describe [Urge Urinary Incontinence⼀Overactive Bladder]
URGE to urinate Suddenly / Overwhelmingly / Frequently

There are 3 types of female Urinary Incontinence
Describe [Overflow Urinary Incontinence]
constant OVERFLOWING DRIBBLE OF URINE and bladder distension 2/2 incomplete bladder emptying

(either from mechanical outlet obstruction or DM Detrusor hypOactivity)
There are 3 types of female Urinary Incontinence
dx for [Overflow Urinary Incontienence] -2
________________
tx for [Overflow Urinary Incontinence] -2
[⇪ post void residual] > 150 cc + neuropathy
________________
[intermittent self catherterization] + [correct underlying etx for incomplete bladder emptying]

If Pap Smear testing reveals [High Grade Squamous intraepithelial lesion], what is the next step in management? -2
COLPOSCOPY = cervix magnified to identify and BIOPSY abnormal areas
________or________
LEEP (loop electrosurgical excision procedure) = excision of cervical transformation zone and surrounding endocervix - [only if done with childbearing]

Trimester WG: [≤13|14-27 | ≥28]
Major causes of [1st trimester ≤14WG] bleeding - 3
- Spontaneous Abortion (inevitable vs threatened)
- Acute cervicitis (postcoital bleeding, Friable cervix with discharge)
- Molar Pregnancy
Differentiate the following spontaneous abortions:
Inevitable abortion
Threatened abortion
Missed abortion
Complete abortion
spontaneous abortion = occurs < 20 WG
- INEVITABLE = vaginal bleeding < 20WG with cervical os dilated –>abortion will inevitably happen soon
* * * - THREATENED = vaginal bleeding < 20WG with cervical os closed is clearly a threat to a STILL LIVING FETUS
* * * - MISSED = retained Fetal death <20WG with cervical os closed…which is why we Missed it - (pt will have pregnancy sx that just suddenly disappear out of nowhere)
* * * - COMPLETE = EXPELED FETAL DEATH <20WG WITH ALL PRODUCTS OF CONCEPTION COMPLETELY EXPELED AND THEN CERVIX CLOSES BACK UP
* spontaneous = occurs < 20 WG*

What are the 3 criteria options for diagnosing
Cervical insufficiency
[pp: ≥2 nonpainful {2nd trimester 14-27WG} spontaneous abortions]
OR
[Cp: Ultrasound showing short cervix ≤25 mm]
OR
[Cp: (early < 24WG ) nonpainful cervical Dilation]
_________________
pp = previous pregnancy
Cp = Current pregnancy
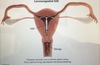
[⬜ placement] ⬇︎ risk of [2T14-27WG] loss in pregnant patients with cervical insufficiency.
What is it called when [pregnancy with cervical insufficiency] fails and prolapses?
and what’s the prognosis for this?
Cerclage;
[Previable Prolapsing amniotic membrane];
POOR PROGNOSIS (PPAM a/w imminent delivery/high risk preterm)
Lactational mastitis occurs ⬜(when?)
as a result of ⬜(etx -6)
[first 3 mo postpartum] ;
[breastfeeding difficulties(improved with lactation consultant)]➜[prolonged breast engorgement(diffuse BL TTP)]
➜ [inadequate milk drainage] ➜[clogged milk ducts & nipple pore]
➜ [Staph A Bacteria(from infant nasopharynx vs Mom skin) retrograde enter nipple pore & divide in stagnant milk]➜ Lactational mastitis
* * *
(**q**[Lies])

Lactational mastitis occurs ⬜(when?)
and presents with what 4 symptoms?
[first 3 mo postpartum] ;
(**q**[Lies])
quadrant[LAD& fever/ induration / erythema / swelling & Pain]