Anatomy - Thorax / Asthma Flashcards
What is the purpose of costal cartilage?
Provides resilience and stability
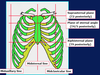
What are these parts called?


What are these lines called?

What are the properties of intercostal muscles?
In intercostal space
3 layers - external, internal, innermost
Respiration importance
Help keep intercostal space rigid
Where is pleura found and what are the 2 types?
Each lung is enclosed in serous pleural sac
2 continuous membranes - visceral (surface) and parietal (inner surface – lines pulmonary cavities)
What are these parts called?


What is a health problem related to the thorax?
Thoracic outlet syndrome - where important arteries and nerves are compressed
What are the 2 thoracic apertures and their function?

What number are these atypical ribs?


What are these parts called?


What is the purpose of the scalene tubercule on rib 1?
Where scalene anterior muscle attaches
Where does the pectoralis major attach to?
Clavicular head which attaches to clavicle
Sternocostal head which attaches to sternum + upper 6 costal cartilages
Fibres which converge on intertubercular groove or humerus
What is the function of the pectoralis major?
- Adductor and medial rotator of arm at shoulder joint
- Can act also as flexor (when arm extended) and as extensor (when arm flexed)
- If pectoral girdle is ‘fixed’, it can act also as an accessory muscle of respiration
Which nerves innervate the pectoralis major?
Medial and lateral pectoral nerves (C5-8 and T1)
Where does the pectoralis minor attach to?
Coracoid process of scapula, ribs 3-5 near cartilage
What is the function of the pectoralis minor?
Depressor of scapula (and, hence, shoulder) and protractor of scapula
If pectoral girdle is ‘fixed’, it can act also as an accessory muscle of respiration
Which nerve innervates the pectoralis minor?
Medial pectoral nerve (C8 and T1)
What are these parts called?


What is the mediastinum?
Central part of thoracic cavity, between pleural cavities
What are the boundaries of th mediastinum?
Sternum (anterior)
Thoracic vertebral column (posteriorly)
Thoracic inlet and root of the neck (superiorly)
Diaphragm (inferiorly)
What are these parts called?


What are the contents superior mediastinum?
- Thymus (lymphoid organ; large between birth and puberty but involutes in adult, especially after disease);
- Great veins (SVC, brachiocephalic vv);
- Phrenic nerves;
- Arch of aorta and branches;
- Origins of internal thoracic arteries;
- Pulmonary aa and vv;
- Vagus nn;
- Recurrent laryngeal branches;
- Trachea (lower half) and bifurcation into main bronchi (T4/5 in expiration); Oesophagus;
- Thoracic duct
What are the divisions are the mediastinum?
Superior and inferior –> behind manubrium sterni and behind body and xiphoid process of sternum
What are these parts called?


What are the contents of the inferior mediastinum?
- Divided into anterior, middle and posterior regions:
- Anterior: Internal thoracic aa and vv (and anterior intercostal branches); thymus (possibly); sternopericardial ligaments
- Middle: Heart and pericardium (serous and fibrous); phrenic nn and pericardiophrenic aa and vv; IVC (diaphragm to right atrium)
- Posterior: Descending aorta (and branches); azygos vv (and tributaries); oesophagus; thoracic duct; sympathetic trunks (and branches)
What are these parts called?


What are these parts called?


What is the purpose of trachea cartilage?
Keeps airways open
What are these parts called?


What are these parts called?


What happens during breathing?
- At rest, diaphragm relaxed
- Muscles of respiration contract to expand thoracic cavity - mainly diaphragm
- This increases thoracic volume / decreases intra-thoracic pressure
- Air drawn into lungs from outside (where pressure greater)
- Air passes into terminal bronchioles / alveoli to oxygenate blood
- Diaphragm relaxes, lungs recoil, thoracic volume decreases, intrathoracic pressure increases and air expelled
What are the properties of the diaphragm?
The most important muscle in respiration
Dome-shaped muscular partition
Separates the thorax and abdomen
Innervated by phrenic nerve – C3-5
Anteriorly attaches into the xiphoid process and costal margin
Laterally attaches to ribs 6-12
Posteriorly attached to T12 vertebra
What does a superior view of diaphragm look like?

What are the properties of intercostal muscles?
- Assist in inspiration and expiration
- Have obliquely angled fibres from rib to rib
- The contraction of External and Internal fibres raises each rib toward the rib above, to raise the rib cage
- Innermost and Internal depresses each rib to the rib below, to lower the rib cage
What are A, B and C?

A = external intercostal muscle
B = internal intercostal muscle (interosseus part)
C = internal intercostal muscle (interchondral part)
What are these parts called?


What are the directions of movement of the sternum and ribs?
Sternum = pump handle movement
Ribs = bucket handle movement

What are the properties of the different types of pleura and lungs?
Pleura = Serous membrane divided into parietal and visceral layers; surround the lungs; contain the pleural cavities; separated by serous fluid
Parietal pleura = Outer; lines thoracic cavity
Visceral pleura = Inner; covers lung following lung fissures
Lungs = Go above 1st rib; covered by suprapleural membrane.
What causes thoracic cavity and lungs to expand?
Surface tension between 2 pleura layers
What are the properties of babies breathing?
- Babies can only breathe via abdominal breathing
- Newborn ribs more horizontal so cant use pump/bucket handle movements
- Intercostals weak
- Abdominal breathing is done by contracting the diaphragm
- As the diaphragm is located horizontally between the thoracic and abdominal cavities, air enters the lungs and the thoracic cavity expands
- Reliance on the diaphragm for breathing means there is a high risk for respiratory failure if the diaphragm is not able to contract
What are the properties of children’s breathing?
- Nasal breathers until 4 – 6 wks
- Short neck & shorter, narrow airways – more susceptible to airway obstruction / respiratory distress
- Tongue is larger in proportion to the mouth - more likely to obstruct airway if child unconscious
- Smaller lung capacity and underdeveloped chest muscles
- Have a higher respiratory rate – newborns ~60 breaths/min, early teens ~20-30 breaths/min
What is a health problem related to breathing?
Harrison’s suculus - defect from rapid breathing causing rib deformation in children
What is the costodiaphragmatic recess?
Where fluid will accumulate in the lungs (look for this abnormality in X-rays)

What does the use of accessory muscles during rest indicate?
Respiratory distress as lungs cannot provide enough oxygen to the body
What is neonatal respiratory distress syndrome?
- Affects premature babies, if they are born before their lungs are fully developed and capable of working properly
- The more premature the baby, the more likely it is that s/he will have respiratory distress syndrome
- Approx. half of all babies born before 28 weeks of pregnancy will develop NRDS
- Leading cause of death in newborns (accounts for 20% of deaths)
What is acute respiratory distress syndrome (ARDS)?
- Fluid / proteins leak from the blood vessels into the alveoli (air sacs)
- Lungs become stiff and so don’t work normally
- Breathing becomes difficult
- Mainly affects people over 75
- Approx 1 in 6,000 people per year affected in England
- Common causes are an infection in the lungs e.g pneumonia
- Lung clots or injury (e.g from a car crash), could also trigger the condition
What are the symptoms of respiratory distress?
Blue extremities
Rapid and shallow breathing
Rapid heart rate
What are the properties of asthma?
Common - ~ 5.4million people in UK receive treatment
An inflammatory disease of the airways of the lungs; persists long-term
- Muscles around the walls of
the airways tighten - so airways
become narrower
- The lining of the airways
becomes inflamed
Variable symptoms - shortness of breath, wheezing, tightness of chest, coughing
What are these parts called?


What is pneumothorax and the 2 types?
- Perforation of parietal pleura = air in pleural cavity
- Tension and non-tension pneumothorax
What is non-tension pneumothorax?
Hole so air in and out, no build-up
Less severe

What is tension pneumothorax?
Air breathed in cannot escape, so remains and builds with each breath
Flap of tissue covers opening
Heart is pushed over - leads to arrythmia

What happens during emphysema?
- COPD
- Over-inflated alveoli so ineffective gas exchange

How is asthma characterised?
Reversible decreases in FEV1:FVC (first expiratory volume in first second and total amount of air expelled)
How is asthma diagnosed?
Variations in PEF which improve with B2 agonist use
What are the properties of COPD?
- Chronic bronchitis and emphysema
- Chronic bronchitis = + airway mucus, airway obstruction and intercurrent infections
- Emphysema = alveoli destruction
- +90% related to smoking
- FEV1 reduced
- Little PEF (peak expiratory flow) variation
What is bronchial calibre control?
Parasympathetic + sympathetic
Sympathetic = circulating adrenaline acting on B2 adrenoceptors on bronchial smooth muscle, causing relaxation
What effect does parasympathetic system have on airways?
- A.Ch. acts on muscarinic M3–receptors:
- Bronchoconstriction
- Increase mucus
What effect does sympathetic system have on airways?
- Circulating adrenaline acting on beta2-adrenoceptors on bronchial smooth muscle to cause relaxation.
- Plus sympathetic fibres releasing NA, acting at adrenoceptors on parasympathetic ganglia to inhibit transmission.
- Beta2-adrenoceptors also on mucus glands to inhibit secretion.
What activates sympathetic nerve?
Irritants, such as dust
Leads to bronchoconstriction
What are the properties of asthma attacks?
Genetic predisposition, provoked by:
Allergens
Cold air
Viral infections
Smoking
Exercise
May be characterised by Early (Immediate) phase followed by Late phase
What do lung function test graphs look like before and after b2 agonist use for someone with asthma?
Decrease in FEV1, reversed by B2 agonist

What are the 3 spasmogens?
- Histamine
- Prostaglandin D2
- Leukotrienes (C4 and D4)
What are 2 chemotaxins and what do they do?
Leukotriene B4, PAF (platelet activating factor)
Lead to late phase
Attract leukocytes (+ eosinophils and mononuclear cells)
Leads to inflammation and airway hyperactivity
What are the 2 pharmacological therapy basis for asthma?
Bronchodilators - reverse bronchospasm in early phase and offer rapid relief
Prevention - prevent attacks, are anti-inflammatory
What are the properties of B2 adrenoceptor agonists?
- Increase FEV1
- Salbutamol
- Increase cAMP on smooth muscle B2-adrenoceptors
- Reduce parasympathetic activity
- By inhalation
- Prolonged use can lead to receptor down-regulation
- Long acting beta agonists (LABA) given for long-term control (i.e. salmeterol)
What is an example of a xathine and its properties?
i.e. theophylline
Bronchodilators, not as good as beta adrenoceptor agonists
Oral or IV in emergency (aminophylline)
Adenosine receptor antagonist
Phosphodiesterase inhibitors

What are examples of muscarinic m-receptor antagonists and their properties?
i.e. ipratropium / tiotropium
Block parasympathetic bronchoconstriction
Inhalation = prevents antimuscarinic side effects
Little value in asthma, used for COPD
What are examples and properties of anti-inflammatory agents?
Preventative
Corticosteroids - i.e. beclomethasone (inhalation) or prednisolone (oral)
Anti-inflammatory = by activation of intracellular receptors, leading to altered gene transcription, less cytokine production, and production of lipocortin/ Annexin A1 (a protein)
What is the function of lipocortin (annexin A1)?
Inhibits prostaglandin and leukotriene synthesis
What are the properties of steroid treatment in asthma?
- Given with B2-agonists
- Reduce receptor down-regulation
- Side effects - throat infections, hoarseness (inhalation) and adrenal suppression (oral)

What is an example and the function of leukotriene receptor antagonists?
i.e. montelukast
+ role as add on therapy
Preventative and bronchodilator
Antagonise actions of leukotrienes
What are the properties of omalizumab?
Role in difficult to treat asthma
Directed against free IgE but not bound IgE
Prevents IgE from binding to immune cells which lead to allergen-induced mediator release in allergenic asthma
What is stepped care and the clinical pharmacology?
Follow guidelines - if salbutamol is used +2 times per week, step up
Spacer devices (patients with – technique and reduce steroid impaction)
Bronchodilator before steroid
Rinse mouth after steroid

What is lung compliance and the properties it in regards to the lungs?
Lung compliance = stretchiness
High pressure = stiffer lung = low compliance
Base of lung = + compliant than apex for better ventilation
Compliance = ensued by elastic recoil
Decreased lung compliance = pulmonary fibrosis, alveolar oedema e.g.
Increased lung compliance = normal ageing lung
Healthy lung = + lung compliance, - alveolar surface tension due to surfactant
What are the 3 lung function tests?
Test mechanical condition of lungs (pulmonary fibrosis)
Test airway resistance (asthma)
Test diffusion across alveolar membrane (pulmonary fibrosis)
What does a spirometer graph tell us?

TV = tidal volume - volume of air entering and leaving the lung with each normal breath
VC = vital capacity - maximum amount of air expelled from the lungs after first filling the lungs to a maximum then expiring to a maximum (TV+IRV+ERV)
IRV = inspiratory reserve volume - extra volume of air inspired above the normal tidal volume with full force
ERV = expiratory reserve volume - extra volume of air expired by forceful expiration at the end of normal tidal expiration

What forced vital capacity (FVC), FEV1.0 and their ratio?
Total volume exhaled
Volume expired in the first second, usually >80% of FVC
FEV1.0 / FVC
What does the helium dilution test test and what are the equations?
Functional residual capacity tests
V1 = known initial volume of helium
C1 = known initial concentration of helium

What does the nitrogen washout test test and how does it work?
- Functional residual capacity
- Patient inspires 100% O2
- Expires into the spirometer system
- Procedure repeated until N2 in lungs is replaced with O2
- FRC calculated from exhaled N2 and estimated alveolar N2

What is restrictive deficit and what diseases does it occur in?
- Lung expansion is compromised - alterations in lung parenchyma, disease of the pleura or chest wall
- Lungs do not fill to capacity hence they are less full before expiration
- E.g. pulmonary fibrosis and scoliosis
- FVC is reduced, but the FEV1.0. is relatively normal
- The FEV1/FVC also remains relatively normal/increased
What is obstructive deficit and when does it occur?
- Characterised by airway obstruction
- If airways are narrowed, lungs can still fill to capacity
- Resistance is however increased on expiration
- E.g. asthma, chronic obstructive pulmonary disease (COPD)
- FEV1.0 will be reduced, but FVC will be relatively normal.
- A low FEV1.0/FVC will be recorded
What is the function of a vitalograph?
Measures ability to move air out of the lungs FVC and FEV1.0
What is the Miller’s prediction quadrant?

What is peak expiratory flow (PEF) recorded as and how does it work?

What do flow-volume loops look like and what type of defecit is the red and orange ones?
Red = restrictive deficit
Orange = obstructive deficit

How do measure PEF and what is gas transfer-diffusion conductance?
Peak flow meter
- Measures how easily CO crosses from alveolar air to blood
- The patient inhales a single breath of dilute carbon monoxide followed by a breath-hold of 10 seconds
- The diffusion capacity is calculated from the lung volume and the percentage of CO in the alveoli at the beginning and the end of the 10s breath-hold
- Clinical relevance - e.g. in fibrosis of the lungs where gas diffusion is compromised

What is the pericardium divided into and what is its function?
Fibrous (outer)
Serous (inner)
Surround the heart
What are the properties of the fibrous pericardium?
- Tough and not distensible
- Attached to diaphragm by pericardiophrenic ligaments
- Blends into adventitia of great vessels
What are the properties of the serous pericardium?
- Comprises visceral layer (epicardium) and parietal layer (lining fibrous pericardium)
- Potential space between them (pericardial cavity)

What do the parietal and visceral pericardial layers line?
Parietal = lines inner surface of fibrous pericardium
Visceral = lines surface of the heart

What are the 4 surfaces of the heart?
Anterior or sternocostal: formed mostly of right (with bit of left) ventricle
Inferior or diaphragmatic: mostly L (with bit of R) ventricle
Posterior or base: mostly L (and bit of R) atrium and pulmonary vv
Pulmonary: mostly L ventricle, in cardiac notch of L lung
What are the 4 borders of the heart?

Superior: from L costal cartilage 2 to R costal cartilage 3
Right: convex to R; from R cc3 to R cc6; mainly R atrium with SVC and IVC
Inferior: lies on diaphragm central tendon; from R cc6 to L intercostal space 5; mainly R ventricle and part of L ventricle
Left: convex to L; from L ics5 and back to L cc2; mainly L ventricle and maybe some L atrium















































































