Condition- Ventricular Tachycardia Flashcards
Define ventricular tachycardia
Regular broad-complex tachycardia rate >120bpm
What causes ventricular tachycardia?
Electrical impulses arising from a ventricular ectopic focus= abnormal excitable group of cells (anothr pacemaker site)
List some risk factors leading to the development of VT
- Coronary heart disease
- Structural heart disease e.g. cardiomyopathies
- Long QT syndrome
- Electrolyte deficiencies (e.g. hypokalaemia, hypocalcaemia, hypomagnesaemia)
- Use of stimulant drugs (e.g. caffeine, cocaine)
List some symptoms of VT
- chest pain
- palpitations
- dyspnoea
- syncope
- +symptoms of cause
List some signs of VT
- Respiratory distress
- Bibasal crackles
- Raised JVP
- Hypotension
- Anxiety
- Agitation
- Lethargy
- Coma
Caused by Congestive cardiac failure
What are the two different types of VT? What causes them?
- monomorphic VT: ECG looks reguar + same shape complexes. Caused by single focal VT/ re-entry rhythm. most commonly caused by MI
- polymorphic VT: All ECG complexes look different. Caused by multiple focal points becoming irritated e.g. in hypoxia
What does this ECG show and why?
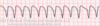
VT= very tidy

Can see AV disocciation (no distinct p waves)
Tachycardia
Broad QRS complex
Other than ECG which other investigations might you conduct on someone with VT?
- Electrolytes
- Drugs and Tox screen
- Cardiac Enzymes (trops)
- TFTs
How would you manage a pt with VT?
- If haemodynamically UNSTABLE:
- DC cardioversion
- Correct electrolyte imbalance
- IV Amiodarone
- If haemodynamically STABLE:
- Amiodarone, Lidocaine, Procainamide
- Correct electrolyte imbalance
- If not corrected: synchronised DC carioversion
How are future VT episodes pevented in a patient who survives?
- Implantable Cardioverter Defibrillator (ICD)
- Radiofrequency ablation of focal points

