Laboratory Tests of Renal Function Flashcards
What contributes towards total body volume?
In health body volume is in a steady state
(this means what goes in should come out)

What does the concentration of any solute in the body depend on?
For any solute, the concentration depends on the amount of the solute present and the volume of solvent (water) in which it is dispersed
What happens if the input of a solute increases and the excreteion stays constant?
The concentration will rise
If the input of a solute decreases and the excretion stays constant, what will happen?
The concentration of the solute will fall
What will happen if the excretion of a solute decreases and the input stays constant?
The concentration of the solute will rise
What will happen to the concentration of solute if the body volume increases and decreases?
If the volume increases due to water overload, the concentration will fall
if the volume decreases due to water deprivation, the concentration will rise
What are the 3 main functions of the kidney?
Excretion:
- the kidneys excrete the end products of metabolism
- e.g. urea from amino acid breakdown
- uric acid from purine (nucleic acid) metabolism
regulation:
- e.g. homeostasis, water, acid base balance
endocrine:
- e.g. renin, erythropoietin
What are some of the homeostatic functions of the kidney?
- Maintenance of water balance by regulating urine volume
- acid base balance by altering hydrogen ion excretion
- sodium balance by altering the rate of sodium reabsorption
What are the endocrine functions of the kidney?
- Secretion of renin from the JGA which influences aldosterone
- erythropoietin effects the rate of red cell production
- 1,25 - dihydroxycholecalciferol is the active form of vitamin D, which affects calcium homeostasis
What types of defects will be seen in patients with chronic renal disease and impaired renal functions?
They show defects in endocrine and excretory functions before the loss of homeostatic control
when homeostatic functions cease, the patient is in renal failure and would die if there were no interventions
What are the purposes of renal function tests?
- They detect renal damage
- They monitor functional damage
- They distinguish between impairment and failure
What is an early test to detect renal damage?
What is a test used to monitor a patient with renal disease?
An early test to detect renal damage is a simple strip test for haematuria - important in screening for heavy metal poisoning
there is a clinical need to monitor a patient with renal disease - this is acheived by serial plasma measurements
About how many nephrons would have to lose their function before tests could detect this?
In renal disease, about half the nephrons have to lose their functioning before the abnormality can be detected by conventional laboratory tests
What are the pre-renal, renal and post-renal causes of kidney failure?
Pre-renal:
- e.g. decreased ECFV or MI
renal:
- e.g. acute tubular necrosis
post-renal:
- ureteral obstruction
What are all the laboratory tests of renal function?
The detection of substances such as red cells or glucose could be an early indicator of renal damage
- glomerular filtration rate
- eGFR - estimate
- creatinine clearance
- plasma creatinine
- plasma urea
- urine volume
- urine urea
- urine sodium
- urine protein
- urine glucose
- haematuria
What is the normal urine volume in health and what does this depend on?
Urine volume depends on how much you drink and sweat
In health it is closely matched to water balance by the hormone ADH, or vasopresssin (AVP)
750 - 2000 mL / 24 hours is typical in health
What is oliguria?
Abnormally low urine volume is a 24 hour volume less than 400 mL
this is oliguria
What is the definition of polyuria?
There is no absolute definition of polyuria as some people can drink an full lot and match it with a high urine output
if the urine volume is greater than 3 litres per day, and the patient is not drinking, this is polyuria
What is the output for anuria?
Anuria is less than 100 mL / 24 hours
What is the reference range for plasma urea?
How sensitive / specific is it?
It provides a quick, simple measurement
it has a wide reference range of 3 - 8 mmol / L
it gives a sensitive but non-specific index of illness
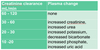
Why is the plasma urea measurement sensitive but non-specific?
The concentration of urea is increased in many different conditions, this makes it sensitive to the presence of disease but a non-specific test
What are the factors influencing plasma urea concentration?


Where is urea filtered?
What % of filtered urea is reabsorbed in health?
Urea is filtered at the glomerulus
about 40% of filtered urea is reabsorbed by renal tubules in health
60% of filtered urea is excreted
How does the amount of urea reabsorbed change with the rate of tubular flow?
The rate of urea reabsorption is variable and depends on the rate of tubular flow
more urea is reabsorbed if the flow rate is slow as there is more time for urea to diffuse into the peritubular capillaries
When does tubular flow rate tend to be slow?
When there is renal hypoperfusion
this may be following myocardial infarction
more urea is reabsorbed and plasma urea increases