Urinary Tract Infections Flashcards
What is the definition of a UTI?
an infection of any part of the urinary system

What is the definition of an infection?
What does infection lead to?
an infection is the invasion of body tissues by a pathogenic organism
this causes an immune response, giving rise to symptoms
What is the most common type of pathogen causing a UTI?
in a UTI, the pathogen is often an endogenous bacteria that has got in the wrong place and invaded
What are the predisposing factors to UTI?
- female sex
- urinary stasis
- urological instrumentation (including catheters)
- sexual intercourse
- fistulae (recto-vesical, vesico-vaginal)
- congenital abnormalities (vesico-ureteric reflux)
What are common causes of urinary stasis?
- pregnancy
- prostatic hypertrophy
- stones
- strictures
- neoplasia
- residual urine from poor bladder emptying
Which areas of the urinary tract are sterile and colonised?
- the kidneys are ureters are sterile
- the bladder is considered sterile, but this may not be the case
- the urethra contains perineal flora

What makes up the perineal flora?
skin flora:
- mainly coagulase negative staphylococci
lower GI tract flora:
- ‘internal’ colonising bacteria are often found on the skin around the relevant orifice
enterobacterales:
- “coliforms” - enteric Gram-negative bacilli
Gram-positive cocci:
- Enterococcus spp.
What endogenous source are most UTIs caused by?
most infections are caused by gut bacteria (enteric flora)
perineum:
- movement of bacteria along a lumen
fistulae:
- movement of bacteria from the genital/GI tract to the urinary tract
What is the other cause of a UTI involving endogenous bacteria?
haematogenous spread
this is the seeding of bacteria to the urinary tract via the blood
e.g. Staphylococcus aureus
this is very rare
What organisms commonly cause UTIs?
- E. coli
- Staphylococcus saprophyticus
- Proteus mirabilis
- Enterococcus spp.
- Klebsiella spp.
- other coliforms
- Pseudomonas aeruginosa

What is the problem with knowing whether a bacteria is the cause of a UTI or whether it is local?
bacteria that cause UTIs can also:
- contaminate poorly taken samples
- colonise catheters
- cause asymptomatic bacteriuria (particularly in >65s)
What is the key to diagnosis in UTIs?
clinical signs and symptoms are the key to diagnosis
AND
microbiology results guide you to the culprit and appropriate, directed treatment
What is seen in asymptomatic bacteriuria?
no symptoms of a urinary tract infection
BUT
cultured urine sample will grow a single organism in significant numbers
What is cystitis?
What are the signs and symptoms?
it is a lower UTI that is more common in women
- dysuria
- frequency
- urgency
- supra-pubic pain or tenderness
- polyuria, nocturia, haematuria
What is pyelonephritis?
What are the signs and symptoms?
an infection of the kidney and/or renal pelvis
symptoms:
- all the symptoms of a lower UTI
- loin / abdominal pain or tenderness
- fever
other signs of systemic infection:
- rigors, nausea, vomiting, diarrhoea
- elevated CRP and WBCs
What are the 2 different types of UTIs?
complicated or uncomplicated
What is the difference between a complicated and uncomplicated UTI?
Complicated UTI:
- underlying abnormailty that is structural or functional
- e.g. urinary stasis - obstruction/retention
- presence of a foreign body
- e.g. catheter / renal calculi / biofilm
Uncomplicated UTI:
- in absence of above
In which types of people should a complicated UTI be suspected unless confirmed otherwise?
children < 10-12
men < 65
what is a catheter-associated UTI?
What are the risks and treatment?
indwelling catheterisation results in bacteriuria
biofilm formation has led to colonisation
manipulation or catheter removal may lead to bacteraemia
antibiotic prophylaxis can be indicated for some patient groups
What types of patient groups would be indicated for antibiotic prophylaxis against a catheter associated UTI?
- previous symptomatic CA-UTI with catheter change/removal
- traumatic catheterisation (including 2 or more attempts)
- purulent urethral/suprapubic catheter exit site discharge
- catheter or meatal/suprapubic catheter exit site colonisation with Staphylococcus aureus (including MRSA)
How is diagnosis of a catheter-associated UTI made?
diagnosis is made by clinical features
there is a need to distinguish between colonisation and infection
dipsticks are no use and “normal” / “sterile” results should not be expected
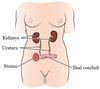
What is a nephrostomy?
an artifical opening created between the kidney and the skin which allows for the urinary diversion directly from the upper part of the urinary system (renal pelvis)
this is performed if there is a blockage in the urinary tract

What are the signs of infection following nephrostomy?
- fever
- pain and tenderness at the site
- haematuria or purulent discharge
What is meant by an ileal conduit / urostomy?
a short section of the ileum is used to drain the ureters directly to a stoma on the anterior abdominal wall after cystectomy
What signs might be seen if there was an infection following ileal conduit / urostomy?
- fever
- ascending infection (upper UTI symptoms)
- para-stomal skin infections - redness, swelling, pus
Why is it important to recognise the symptoms of infection following nephrostomy or ileal conduit?
like catheters, colonisation of the tubing and bags occurs


