Inflammatory Skin Pathology & Skin Tumours Flashcards
What are the 2 categories of inflammatory skin disease and examples?
infectious
non-infectious inflammatory diseases:
- dermatitis / psoriasis
- blistering
- connective tissue diseases
- e.g. lupus erythematosus / dermatomyositis
- skin lesions as a sign of systemic disease
- skin lesions caused by metabolic disorders
plus some rare types
How common is eczema / dermatitis?
How severe it is?
it is very common and affects 5% of children in UK
it varies from trivial to severe
it is a reaction pattern rather than a specific disease
What are the 3 clinical stages of dermatitis (eczema)?
1. acute dermatitis:
- red skin, weeping serous exudate +/- small vesicles
2. subacute dermatitis:
- red skin, less exudate, lots of itching, crusting
3. chronic dermatitis:
- skin is thick and leathery secondary to scratching
What are the 3 things seen in the microscopy in dermatitis?
spongiosis:
- intercellular oedema within epidermis
chronic inflammation:
- predominantly superficial dermis
epidermal hyperplasia & hyperkeratosis:
- mild in acute dermatitis
- marked in chronic dermatitis
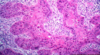
What is visible in this image?

spongiosis in eczema
What is atopic eczema?
When does it occur?
it is a type 1 hypersensitivity reaction to an allergen
it usually starts in childhood, but occasionally occurs in adults
there is often a family history and it is often associated with asthma and hay fever
What are the 2 types of contact dermatitis?
What causes them?
contact irritant dermatitis:
- direct injury to skin by an irritant
- e.g. acid, alkali, strong detergent
contact allergic dermatitis:
- e.g. nickel, dyes, rubber
- act as haptens which combine with epidermal protein to become immunogenic
What are the morphological subtypes of dermatitis of unknown aetiology?
seborrhoeic dermatitis:
- affect areas rich in sebaceous glands
- e.g. scalp, forehead, upper chest
nummular dermatitis:
- coin shaped lesions
What is psoriasis?
What % of the population are affected?
well defined, red oval plaques on extensor surfaces (knees, elbow, sacrum)
they have a fine silvery scale and Auspitz sign
removal of the scale causes small bleeding points
+/- pitting nails, +/- sero-negative arthritis
affects 1-2% of the population
What are the microscopic features of psoriasis?
“psoriasiform hyperplasia” has a distinct appearance:
- regular elongated club shaped rete ridges
- thinning of epidermis over dermal papillae
- parakeratotic (contain nuclei) scale
- collections of neutrophils in scale (Munro microabscesses)
What is the pathogenesis of psoriasis?
the clinical and microscopic features reflect massive cell turnover
What is shown here?

psoriasis

What are the genetic factors and environmental trigger factors involved in the aetiology of psoriasis?
genetic factors:
- some have family history
- multiple loci (psoriasis susceptibility or PSORS genes) with many in the region of MHC on chromosome 6p2 implicated
- this is the same area involved in other autoimmune disorders
environmental trigger factors:
- these are acquired factors
- infection, stress, trauma, drugs
What is the associated comorbidity in psoriasis?
- arthropathy (disease of the joints) associated in 5-10% cases
- psychosocial effects
- cardiovascular disease increased risk by 2-3 x
- cancer - increased risk of non-melanoma skin cancer & lymphoma
What are the 2 different types of lupus erythematosus?
discoid LE
- affects the skin only
systemic LE
- this is a visceral disease that may or may not involve the skin
What does lupus erythematosus look like clinically?
- red scaly patches on sun-exposed skin +/- scarring
- scalp involvement causes alopecia
- butterfly rash on cheeks and nose in SLE
What is lupus erythematosus?
What body parts can it affect?
an autoimmune disorder primarily affecting connective tissues of the body
autoantibodies are directed at various tissues
it may affect any part of the body, but importantly kidneys
What does lupus erythematosus look like microscopically?
thin, atrophic epidermis with inflammation and destruction of adnexal structures
IMF - LE band
IgG deposited in basement membrane
How does systemic lupus erythematosus (SLE) affect the body?
- 30% CNS involvement
- 50% butterfly erythema
- 50% pleuropericarditis
- 50% renal involvement
- 20% discoid skin involvement
- 90% arthralgia, arthritis
- 80% common symptoms (fever, fatigue)
- 70% vasculitis / skin involvement

what is shown here?

lupus erythematosus
What technique is used to detect lupus erythematosus?
immunofluorescence
What is dermatomyositis?
what test can be performed?
peri-ocular oedema and erythema (Heliotropic rash)
erythema in photosensitive distribution
myositis - proximal muscle weakness
(can check for creatinine kinase)
25% cases are associated with underlying visceral cancer
What is a heliotropic rash?
reddish purple rash on or around the eyelids
it is often accompanied by swollen eyelids
What does the microscopy look like in dermatomyositis?
- similar to lupus erythematosus
- often a lot of dermal mucin
- negative IMF
What are bullous diseases?
formation of fluid filled blisters
What is the difference between pemphigus and pemphigoid?
pemphigus:
- affects the outer layer of the skin (epidermis)
- causes lesions and blisters that are easily ruptured
pemphigoid:
- affects a lower layer of the skin, between the epidermis and the dermis
- causes tense blisters that do not break easily

What is pemphigus?
What types of blisters does it involve in?
group of disorders characterised by loss of cohesion between keratinocytes resulting in an intraepidermal blister
all types cause fragile blisters / bullae which rupture easily
can be extensive +/- involve mucous membranes
What is the pathogenesis of pemphigus?
autoantibodies directed against intercellular material
can be detected by immunofluorescence (IMF)
What is bullous pemphigoid?
What are the blisters like?
a disease characterised by subepidermal blisters
elderly with large tense bullae which do not rupture easily
it can be localised or extensive disease
What is the pathogenesis of bullous pemphigoid?
autoantibodies to glycoprotein in the basement membrane
it can be detected by IMF