First Aid Microbiology 3 Flashcards
Condylomas

The limited list of rashes that may appear on palms of hands and soles of feet

What is this finding on CT angiography? (It has a correlate on gross pathology)
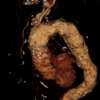
Tree bark aorta
Named for its appearance. This is a characteristic of tertiary syphilis, and is a form of ascending thoracic aortic aneurysm.
The pathology is due to invasion of the vasa vasorum (vessels of the vessel) that supply the thick muscular walls of the aorta.
What is going on in this infant with the displayed findings?

Congenital syphilis
Characteristic findings: Tooth abnormalities, saddle nose, perioral fissures, congenital deafness, high arched palate, and joint separation in feet and sometimes arms.
Treating syphilis
Always treat w/ penicillin
If Jarisch-Herxheimer reaction evolves, simple supportive care, NSAID analgesia, and potentially benzodiazepine sedation are all that will be necessary – it is self limited.
The two diseases caused by Legionella
Pontiac fever and Legionaire’s Disease
Pontiac fever is an acute, nonfatal respiratory disease. It causes a mild upper respiratory infection that resembles acute influenza. Pontiac fever resolves spontaneously and often goes undiagnosed.
Legionaire’s Disease is a severe pneumonia associated with hyponatremia, diarrhea, and neurologic symptoms that usually occurs in smokers and can spread in epidemic fashion.
Both are treated with fluoroquinolones or macrolides.
Why is pseudomonas SO BAD for CGD patients?
It is encapsalted as well as both catalase positive and oxidase positive
What is going on in this individual’s foot?

This is a not uncommon clinical scenario.
Diabetic neuropathy predisposes diabetic patients to these foot ulcers. These ulcers are then at risk for subsequent infections, and one of the major offenders is Pseudomonas aeruginosa. P. aeruginosa is so bluish-green that it can literally color the wound site, making it apparent that it should be at the top of your differential in cases like this.
P. aeruginosa is also the most common cause of osteomyelitis in diabetic patients.
What is the #1 most common and most feared infection in a burn patient?
Pseudomonas aeruginosa
Patient presents to primary care with the following presentation. They report that they are up to date on their vaccination status and have been quarantining at home. They have been spending much of their time enjoying their home built hot tub which was recently finished.
What is the likely causative organism? How could this have been avoided?

This is hot tub folliculitis
It is caused by Pseudomonas aeruginosa, and is prevented from developing in hot tubs and swimming pools by adding chlorine to the water.
Patient with PMH notable for diabetes presents with subacute hearing loss and painful inflammation of the external ear. The following is observed upon speculum exam.
The most likely causative organism for this patient’s disease shares a toxin with what other deadly bacterium? How does the toxin work?

This patient most likely has Pseudomonas aeruginosa infection of the external ear.
Pseudomonas shares a toxin with Corynebacterium diphtheriae which works by ribosylating EF2 and preventing protein translation in mammalian cells, leading to cell deaths
What can kill Pseudomonas?
Piperacillin (penicillinase-resistant penicillin)
Aminoglycosides
Fluoroquinolones
Patient presents with cellulitis of the forearm following being bitten by their pet dog at this site the previous day. What is the likely causative organism?
Pasteurella multocida (think Pasteur’s pet dog Ella)
Note that this could easily have been a cat too, but it would have to be a bite, not a scratch (like for Bartonella). The organism lives in the respiratory tracts of dogs and cats.
Like Pseudomonas, Pasteurella are catalase positive, oxidase positive, and encapsulated, making them a nightmare for patients with CGD.
It displays bipolar “safety pin” staining. Treat w/ amoxicillin-clavulonate.

On laboratory testing, the bacteria associated with an individual’s sputum sample are found to be lacking a component of peptidoglycan called muramic acid.
What is the likely causative organism for their pneumonia?
Chlamydophila pneumoniae
Lack of muramic acid in the cell wall is a defining characteristic of the chlamydia and chlamydophila species. It also means that they are resistant to penicillins.
So, treat w/ macrolides. If C. trichomatis, then assume N. gonorrheae is also present and give ceftriaxone too.
When dealing with gram intermediate bacteria with complex life cycles, the ___ form is always the infectious form and the ___ form is the noninfectious form which can divide.
When dealing with gram intermediate bacteria with complex life cycles, the elementary form is always the infectious form and the reticulate form is the noninfectious form which can divide.
Reticulate means to divide!
Organisms that stain w/ Giemsa
- Borrelia (Lyme)
- Chlamydia species
- Klebsiella granulomatis (Donovanosis)
- Amoebic parasites:
- Plasmodium species (Malaria)
- Pneumocystis jirovecii
- Babesia species (Babesiosis)
Subgroups of Chlamydia trichomatis and what they cause
- A-C: Blindness
- D-K: STI
- L1-L3: Lymphogranuloma venerium (LGV)
Patient presents w/ genital infection. You suspect a common STI based on the clinical history.
How do the characteristics of the discharge of the wound influence your suspicion of the causative organism?
If the discharge is thick and purulent, it is more likely to be Neisseria gonorrheae
If the discharge is watery, it is more likely to be Chlamydia trichomatis
Note that either way, your treatment regimen will assume that both organisms are present, since they are often co-infectious.









