Viral and Fungal Infections Flashcards
Incubation and shedding duration of influenza
Incubation: 1-4 days
Shedding: 0-10 days
3 antivirals for influenza
Oseltamivir
Zanamivir (inhaled)
Peramivir (IV)
Antiviral in influenza not recommended in asthma/COPD
Zanamivir
Difference between CMV infection and CMV disease
Infection: lab confirmed virus, regardless of signs/symptoms
Disease: signs and symptoms of disease
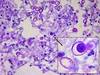
Most common forms of aspergillus in humans
Aspergillus fumigatus
Aspergillus flavus
Clinical spectrum after aspergillus spore inhalation

Fungal tests affected by antibiotics
Beta Glucan and Galactomannan (also by pasta and rice)
First line treatment of invasive pulmonary aspergillosis
Voriconazole
Drug for IPA prophylaxis in AML, MDS, and GVHD
Posaconazole
Medications to treat chronic necrotizing pulmonary aspergillosis
Voriconazole
Itraconazole
Ampho B
Caspofungin
Treatment options for aspergilloma
Observation if asymptomatic
Itraconazole (only 60% effective)
Surgical resection
Bronchial artery embolization
Criteria for ABPA
Must have either asthma or CF
Aspergillus skin test or IgE against A. fumigatus
TOTAL IgE > 1000
Treatment for severe blastomycosis
Ampho B 1-2 weeks, then itraconazole
Treatment for mild to moderate blastomycosis
Itraconazole 6-12 months
Treatment for blasto with CNS disease
Ampho B