Cervical Screening / Vulval Pathology Flashcards
(46 cards)
identify the cells present within normal ectocervix?

what does the endocervix normally look like histologically?

what is the transformation zone and which physiological changes causes the altering of position of TZ during life?
squamo-columnar junction between ectocervical (squamous) and endocervical (columnar) epithelia
position of TZ alters in response to menarche, pregnancy and menopause
what does the squamo-columnar junction look like histologically?
what is cervical erosion?
the exposure of delicate endocervical epithelium to acid environment of vagina leads to physiological squamous metaplasia
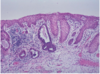
what are nabothian follicles?
mucous filled cyst on surface of cervix - formed when stratified squamous epithelium of ectocervix (nearest vagina) grows over columnar epithelium of endocervix (portion nearest to uterus)
what are the symptoms and causes of cervicitis?
often asymptomatic but can lead to infertility due to simultaneous sildent fallopian tube damage
causes - non specific inflammation, follicular cervicitis (sub epithelial reactive lymphoid follicles present in cervix), chlamydia and HSV
what is a cervical polyp and what is the main symptom?
localised inflammatory outgrowth (not premalignant)
cause of bleeding, if ulcerated
what are the different neoplastic causes of cervical pathology?
cervical intraepithelial neoplasia (CIN)
cervical cancer = squamous carcinoma, adenocarcinoma
what are the risk factors for CIN / cervical cancer?
high risk HPV esp 16 and 18 (sexual partners may increase risk)
vulnerability of SC junction in early reproductive lise - age at first intercourse, long term use of OCP, non use of barrier contraception
smoking - 3x risk
immunosuppression
what strains of HPV causes genital warts and what does this look like histologically?
HPV 6 and 11
condyloma acuminatum = thickened “papillomatous” squamous epithelium with cytoplasmic vacuolation (koliocytosis)
what strains of HPV causes cervical intraepithelial neoplasia (CIN) and what does this look like histologically?
HPV 16 and 18
infected epithelium remains flat, but may show koilocytosis, which can be detected in cervical smears

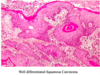
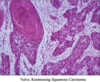
what does cervical cancer look like histologically?
invasive squamous carcinoma - virus integrated into host DNA
how long does it take for HPV infection to progress to high grade CIN?
6 months - 3 years
how long does it take for high grade CIN to become invasive cancer?
5-20 years
what does mild dyskaryosis with viral features (HPV) look like?

what is cervical intraepithelial neoplasia (CIN) and where does it occur?
pre-invasive stage of cervical cancer - dysplasia of squamous cells which is not visible by naked eye and is asymptomatic
occurs at transformation zone
detected by cervical screening
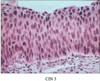
describe the progressive degrees of dysplasia and neoplasia of cervix?
normal squamous epithelium -> koilocytosis -> CIN1 -> CIN2 -> CIN3

describe the general histology of CIN?
delay in maturation / differentiation (immature basal cells occupying more of epithelium)
nuclear abnormalities (hyperchromasia, increased nucleocytoplasmic ratio, pleomorphism)
excess mitotic activity (situated above basal layers, abnormal mitotic forms)
often koilocytosis (indicating HPV) also present, CIN is graded I-III
descrbe the histology of CIN I?
basal 1/3 of epithelium occupied by abnormal cells
*raised numbers of mitotic figures in lower 1/3
*surface cells quite mature, but nuclei slightly abormal

describe the histology of CIN II?
abnormal cells extend to middle 1/3
*mitoses in middle 1/3
*abnormal mitotic figures

describe the histology of CIN III?
abnormal cells occupy full thicknes of epithelium
*mitoses, often abnormal, in upper 1/3
75-95% of malignant cervical tumours are what kind?
invasive squamous carcinoma (2nd most common female cancer worldwide)
*develops from CIN - preventable by screening
what are the different stages of invasive squamous carcinoma?
stage 1A1 - depth up to 3mm, width up to 7mm
stage 1A2 - depth up to 5mm, width up to 7mm (low risk of lymph node metastases)
stage 1B - confined to the cervix
stage 2 - spread to adjacent organs (vagina, uterus, etc)
stage 3 - involvement of pelvic wall
stage 4 - distant metastases or involvement of rectum or bladder