Chapter 13 - Blood vessels Flashcards
(130 cards)
Review:
What is the intima?
What is the media?
What is the adventitia?
How are they supplied?
-
Intima
- Single layer of endothelial cells with little subendothelial CT
- Supplied by the lumen
- Separated from media by the internal elastic lamina
-
Media
- Smooth muscle
- Inner layers: lumen
- Outer layers: small arterioles (vasa vasorum)
-
Adventitia
- CT, Nerves, and Vasa Vasorum
Review
Difference between large, medium, and small arteries?
- Large (elastic arteries)
- Media = rich in elastic fibers that alternate with layers of smooth muscle
- Medium (muscular arteries)
- Media = mostly smooth muscle
- Small (less than 2mm)
- Structurally similar to medium arteries
- Found within tissue and organs
Review still:
Arterioles:
Composition?
Importance?
Capillaries:
Composition?
Importance?
- Arterioles
- Small amount of smooth muscle
- NO elastic lamina
- *Principle sites of BF resistance*
- Capillaries
- Endotheilal lining but NO media
- BF slows dramatically here obbbbbviously for nutrient exchange
Review:
Where does blood flow after capillaries? What is important about these?
Veins in comparison to arteries?
Composition of lymphatics?
- Postcapillary venules (after cap)
- Site of inflammation induced leakage
- Veins
- Large lumens and walls (less organized than art.)
- Contains 2/3 of all blood
- Lymphatics
- Thin-walled, endotheium lined channels
- Drain intersitial fluid and inflammatory cells
How are endothelial cells identified immunohistochemically?
Endothelial cells identified by:
- PECAM-1 (CD31)
- CD34
- vWF
Functions of endothelial cells?
Endothelial cell function:
- Maintenance of permeability barrier
- Elaboration of compounds that control coagulation
- Produce ECM proteins for healing/angiogenesis
- Production of vasoconstrictors (endothelin/angiotensin)
- Production of vasodilators (NO/prostacyclin)
- Important mediators of inflammation
- Produce IL-1/6/8
- Express VCAM-1, ICAMS, E/P selectin
- Produce growth factors
What is endothelial dysfunction associated with?
Endothelial dysfunction:
- Abnormal thrombus formation
- Atherosclerosis
- Vascular lesions of hypertension
Functions of vascular smooth muscle cells?
Vascular smooth muscle cells:
- Vasodilation/constriction in response to mediators
- Synthesis extracellular basement membrane proteins
- Collagen, elastin, and proteoglycan
- They can also proliferate and be migratory
- In response to cytokines (IL-1, IFN)
- In response to GF (PDGF, endothelin-1, and FGF)
What layer of the artery thickens in response to vessel injury?
The intima
What is the pathology of intimal thickening in response to vessel injury?
Pathology
- Endothelial cells lose the ability to contract but they proliferate and produce ECM proteins, creating what is known as the neointima*
- If chronic - associated with atherosclerosis
Arteriosclerosis:
Generic term for?
What are the 3 variations?
Arteriosclerosis:
- Arterial wall thickening and the loss of wall elasticity
3 variations:
- Monckeberg medial calcific sclerosis
- Arteriolosclerosis
- Atherosclerosis
What is monckeberg medial calcific sclerosis?
Characterized by excessive Ca++ deposits in muscular arteries (50+ yo) that are usually benign because the deposits do not cause obstruction
What is arteriolosclerosis?
Involves arterioles and small arteries
Hyaline and hyperplastic forms occur and are associated with thickening of the vessel walls and obstruction of the lumen
What is atherosclerosis characterized by?
Characterized by intimal lesions known as atheromas or atheromatous fibrofatty plaques
(they may obstruct the lumen and weaken the media)
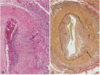
What is this an example of?

This is Monckeberg medial calcific sclerosis with the collection of calcium deposits (arrows) in the media of small muscular arteries
Where do atherosclerotic lesions primarily develop?
Atherosclerotic symptomatic disease most often involves the arteries supplying what organs?
- Lesions develop in:
- Elastic arteries (aorta, carotid, and iliac)
- Large/medium muscular arteries (coronary/popliteal)
- Symptomatic disease involves arteries supplying:
- Heart
- Brain
- Kidneys
- Lower extremities
Major outcomes of atherosclerosis?
Atherosclerosis major outcomes:
- MI
- Stroke
- Aortic aneurysms
- Peripheral vascular disease
Earliest lesion of atherosclerosis
Earliest lesion:
- Fatty streaks in the intima
- Lipid filled macrophages (foam cells)
- Not raised so no disturbance in BF
Atherosclerotic plaques typically have what 3 principal components?
- Cells
- Smooth muscle, macrophages, and lymphocytes
- ECM proteins
- Collagen, elastic fibers, and proteoglycan
- Intra/Extracellular Lipid
- Cholesterol clefts are common
Top risk factors for CVD?
- Hyperlipidemia
- Hypertension
- Cig smoking (oops)
- Diabetes
- Advanced age
Response to injury hypothesis implies?
Implies that atherosclerosis is a chronic inflammatory response of the artery wall initiated by injury to the endothelium
Lesion progression of atherosclerosis is sustained by?
Sustained by interactions between
- lipoproteins
- Macrophages
- T cells
- Smooth muscle cells
Steps in lesion development?
- Chronic injury
- Accumulation of lipoproteins (mostly LDL)
- Increased adhesion of monocytes/leukocytes to endo.
- Adhesion of platelets
- Release of factors that induce smooth muscle migration
- Smooth muscle proliferation
- Elaboration of extracellular matrix proteins
What is C-reactive protein?
CRP = one of the cheapest and most sensitive predictors of the risk of MI, stroke, peripheral arterial disease, and sudden cardiac death