CNS Blood Supply COPY Flashcards
(435 cards)
What proportion of CO is received by brain?
What proportion of O2 does it use?
17%
20%
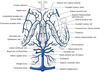
Describe the intracranial course of the carotid artery
Enters the skull in the middle cranial fossa beside the dorsum sellae of the sphenoid.
Carotid siphon- anterior, superior at medial ACP, enters subarachnoid space and courses posteriorly below optic nerve turning upwards lateral to optic chiasm
Divides into terminal branches below anterior perforated substance

Which artery supplies the neurohypophysis?
Inferior hypophyseal

What do the superior hypophyseal arteries supply?
Enter the median eminence of the hypothalamus.
Break up into capillary loops into which hypothalamic releasing factors gain access.
The capillary loops drain through small hypophyseal portal veins into the capillaries of the anterior lobe.

Where is the ophthalmic artery given off?
Immediately after the ICA enters the subarachnoid space
What structures are supplied by the ophthalmic artery?
Eye and other orbital contents
Frontal area of the scalp
Frontal and ethmoid paranasal sinuses
Parts of the nose
What are the branches of the ophthalmic artery?
DR MCLESSI
D: dorsal nasal artery
R: (central) retinal artery
M: muscular artery
C: ciliary arteries (long, short and anterior)
L: lacrimal artery
E: ethmoidal arteries (anterior and posterior)
S: supraorbital artery
S: supratrochlear artery (frontal artery)
I: internal palpebral artery

Which of the branches of the ophthalmic artery supply the nose?
Anterior and posterior ethmoidal
Passage of the anterior choroidal artery
Posterior- along optic tract, choroid fissue at medial edge of temporal lobe
Branches to optic tract, uncus, amygdala, hippocampus, globus pallidus, lateral geniculate body and ventral part of the internal capsule.
Terminal branches→ choroid plexus in temporal horn anastomosing with posterior choroidal

Neurological deficit with ICA occlusion
Blindness of ipsilateral eye
Loss of contralateral half of visual field.
Contralateral hemiplegia and hemianopia with global aphasia
Neurological deficit with anterior choroidal occlusion
Contralateral hemiplegia and sensory abnormalities (internal capsule)
Contralateral homonymous heminaopia
Passage of MCA
Runs deep in the lateral sulcus between the frontal and temporal lobes


What branch of the ACA is given off just proximal to the AComm?
Medial striate artery (recurrent artery of Heubner)

What is supplied by the recurrent artery of Heubner?
aka Medial striate artery
Penetrates the anterior perforated substance to supply the ventral part of the head of the caudate nucleus, the adjacent part of the putamen and the anterior limb and genu of the internal capsule

Branches of the ACA
Ascends in the longitudinal fissure and bends backwards around the genu of the corpus callosum.
Supplies medial part of the orbital sufrace of frontal lobe including the olfactory bulb and tract.
Continues along the upper surface of the corpus callosum as the pericallosal artery and a large branch, the callosmarginal artery follows the cingulate sulcus.

Why does a unilateral MCA lesion cause no loss of hearing even though the auditory cortex is including in the MCA territory?
Due to the bilateral cortical projection.
Why does a lesion in the internal capsule not cause aphasia?
Because the connections of the language areas with the contralateral hemisphere are intact.
Features of anterior cerebral artery occlusion
Contralateral paralysis of leg and perineum.
May have urinary incontinence caused by inadequate perineal sensation.
May also have contralateral facial weakness due to corticofugal fibres.
Infarction of olfactory lobe may cause anosmia.
Mental confusion and dysphasia may result ?due to loss of function in the prefrontal cortex, cingulate gyrus and SMA
How does the vertebral artery enter the subarachnoid sapce?
Pierces the atlanto-occpital membrane then the arachnoid and dura mater at the foramen magenum
Whence does the single anterior spinal artery arise?
From a contribution from each vertebral artery.
From what do the posterior spinal arteries arise
Either as a branch of the vertebral or PICA.
Passage of PICA
Irregular course between medulla and cerebellum.
Branches of PICA
Distributed to posterior parts of the cerebellar hemisphere, inferior vermis, central nuclei of cerebellum and choroid plexus of the fourth ventricle.
There are also important medullary branches to the dorsolateral medulla