Course 2: Pathophysiology Flashcards
(200 cards)
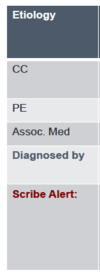
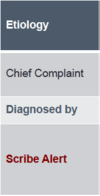
Example Pathophysiology (ED Flow)

Differential Diagnosis
1. Differential Diagnosis: the different diseases the physician comes up with to explain the true source of the pc’s chief complaint
- associated symptoms, associated meds, PE findings, and diagnosis of diseases are all methods used to condirm the differential diagnosis

Pertinent Positives
specific symptoms that raise the physician’s suspicion for a particular disease
Pertinent Negatives
specific symptoms that are not present which cause teh physician to doubt certain diagnosis


Coronary Artery Disease
(Etiology)

CAD

Myocardial Infarction
(Etiology)
-
MI:
- STEMI—» ST elevation present (EKG)
- non-STEMI—» happened recently but non-ST elevated MI (troponin lvls)

Congestive Heart Faliure
(Etiology)

- CHF
- heart becomes enlarged, inefficient, and congested with excess fluid
- PE:
A) rales (snap, crackle, pop sound in lungs upon breathing),
B) Jugular Vein Distention (JVD) in neck,
C) pitting pedal edema ( Observable swelling of body tissues due to fluid accumulation that may be demonstrated by applying pressure to the swollen area)

Atrial Fibrillation
(Etiology)

- AFIB
- electrical abnormalities in the “wiring” of the heart causes the top of the heart (atria) to quiver abnormally

what are 3 Shortness of Breath (SOB) Symptoms associated with CHF?
- worse with lying flat (Orthopnea)
- paroxysmal nocturnal dyspnea (PND)
- Dyspnea on Exertion (DOE)
inflammation of the sac surrounding the heart causing CP (chest pain)
Pericarditis
inflammation of the sac surrounding the lungs causing pleuritic CP
Pleurisy
irritation of the ribs causing CP worsened by pressing on the sternum
Costochondritis
irritation of the chest wall causing pain with palpation of the chest
Chest Wall Pain
fluid collecting around the lungs causing SOB or CP
Pleural Effusion
Cardiovascular Summary Slide
- Diagnosis
- What is it?
- Diagnosed by what tests?


Pulmonary Embolism
(Etiology)

- PE
- a blood clot disloges from pulmonary artery and blocks blood flow to the lungs

Pneumonia
(Etiology)

- PNA
- infiltrate (bacterial infection) and inflammation within the lung

Pneumothorax
(Etiology)

- PTX
- collapsed lung due to trauma or a spontaneous small rupture of the lung

Chronic Obstructive Pulmonary Disease
(Etiology)

- COPD
- long-term damage to lung’s alveoli (emphysema) along w/inflammation and mucus production (chronic bronchitis)

Asthma (Reactive Airway Disease)
(Etiology)

- Asthma
- constricting of the airway due to inflammation and muscular contraction of the bronchioles (i.e. bronchospasm)

Pulmonary Summary

- Diagnosis
- catch phrase?
- Diagnosed by…?

Ischemic Cerebrovascular Accident
(Etiology)

- CVA
- blockage of the arteries supplying blood to the brain resulting in permanent brain damage

Transient Ischemic Attack
(Etiology)
- TIA
- vascular changes temporarily deprive part of the brain from oxygen—»symptoms generally last less than 1 hr