developmental aspects of lung disease Flashcards
(50 cards)
5 stages of lung development
embryonic, pseudoglandular, canalicular, saccular, alveolar
between what age is embryonic lung development
3-8wks
between what age is pseudoglandular lung development
5-17wks
between what age is canalicular lung development
16-26wks
between what age is saccular lung development
24-38wks
between what age is alveolar lung development
36wks-2/3yrs
embryonic lung development
lungs appear as offshoot from the oesophagus no clear cell differentiation yet ridge develops between oesophagus and trachea, lung buds continue to develop off, lobes can be seen developing
pseudoglandular lung development
progressive spreading of the bronchi, conducting system begins to form as sections of the lung begin to divide off cilia develop around wk 13
canalicular lung development
early gas exchange structures form lung becomes increasingly vascularised which is important in its overall development type I and II pneumocytes begin to differentiate structures involved in surfactant production are produced
saccular lung development
further evolution of the gas exchange structures type I and II pneumocytes become visible thinning out of areas for gas exchange
alveolar lung development
usually occurs after the child is born sacuoles change in shape, geometry and function after birth and continue to grow over the next 3-12 yrs
post-natal lung growth
alveolar septation continues 100-150mln at birth to 200-600mln at 3-8yrs increased alveolar dimensions thereafter anything that affects the amount of alveoli you have in early life will have a knock on effect later on
common upper (tracheo-bronchial) congenital abnormalities
tracheal agenesis and stenosis tracheomalacia tracheo-oesophageal fistula (relatively common)
common lower (broncho-pulmonary) congenital abnormalities
lung agenesis/pulmonary hypoplasia bronchogenic cyst, CPAM (sporadic malformations) congenital diaphragmatic hernia
how are congenital abnormalities diagnosed
antenatally newborn childhood asymptomatic - incidental finding
presenting features antenatally
US scan 12 wk dating scan - abnormalities are more likely to be picked up at 20wks fluid amount can indicate problems w/ lungs or gut can do MRI to look for specific problems
newborn presenting features
tachypnoea respiratory distress feeding issues - e.g. can’t breathe and feed at the same time
childhood presenting features
recurrent symptoms stridor/wheeze (wheeze is usually monophonic) recurrent pneumonia (structural abnormality predisposes them) cough feeding issues
how would CPAM appear on fetal imaging
white as it is often a cystic abnormality
tracheal agenesis
very rare presents at birth with acute respiratory distress and inability to intubate usually diagnosed before birth

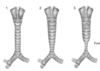
tracheal stenosis
very rare complete cartilage rings - may be generalised or segmental present at birth or within first year 3 types, increasing narrowing of trachea, funnelling can create blockages
tracheomalacia
more common floppiness of the airway dynamic abnormal collapse of tracheal walls closes readily during expiration, can be a problem during infection C shaped appearance in the back wall can be isolated in healthy infants

what is tracheomalacia caused by
associated with genetic conditions may be caused by external compression e.g. vessels, tumour
tracheomalacia presentation
barking cough recurrent croup SOB on exertion stridor/wheeze noisy in their regular breathing







