Disease of Kidneys I - Nephritic Flashcards
(52 cards)
What is generally seen in nephrotic syndrome?
proteinuria (>3.5 mg/day; foamy/frothy urine); hypoalbuminemia (dec oncotic pressure-> edema); severe edema; hyperlipidemia; lipiduria
Define azotemia.
acute renal failure resulting in an increase in nitrogenous wastes in blood (BUN, creatinine) - exists WITHOUT clinical symptoms but can progress to chronic renal failure
What are some causes of azotemia?
prerenal (decreased blood flow), post renal (ureter obstruction), intrarenal (tubular necrosis or interstitial nephritis)
What is uremia?
chronic renal failure : azotemia + clinical manifestations
What are the 3 general cell types in glomerulus?
podocytes (renal epithelial cells), vascular endothelial cells, mesangial cells
Where are neoplastic changes usually found?
tubular epithelial cells (since there’s regenerative capacity)
Endothelial cells line _____.
vascular spaces
Podocytes line _____.
urinary space
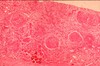
What is seen histological in normal glomerulus?
one mesangial cell nucleus, mesangial matrix, endothelial and epithelial cells
BM thin and delicate with uniform thickness
Capillary lumens open
Tubule epithelial cells back-to-back -> interstituim is not thickened
What is significant about the width of podocyte foot processes at EM?
same width as BM
Why is fluorescent microscopy essential for diagnoses?
usu H&E not enough to determine pathology
essential to detect immune complexes
Name and describe 2 patterns of pathology seen on fluorescent microscopy.
- homogenous staining: thin, delicate BM -> uniform ribbon staining reflective of autoimmune anti-BM disease
- granular aspect: lots of deposits; representative of thousands of immune complexes (“dense, strings of pearls look”

What is seen generally in acute nephritic syndrome?
hematuria (“red urine); glomerular hypercelluarity; RBC casts in urine; diminished GFR; mild to moderate proteinuria; HTN; azotemie; oliguria
associated with acute onset
What is another name for acute nepritic syndrome?
acute glomerulonephritis
How do RBC casts form?
as the RBC cross the BM, the rate of flow in the tubules slow down -> RBCs start sticking together and forming a cast
Tubules produce protein matrix on the cell membrane surfaces -> causes stickiness within tubules
when flow restored -> washed out in urinalysis!
What are RBC casts indicative of?
urinary tract damage in kidneys - nephritic
What do WBC casts indicate?
tubular inflammatory/infectious diseases of kidneys
What’s another name for acute proliferative glomerulonephritis?
Post-infection, Post-streptococcal
Is acute proliferative glomerulonephritis nephritic or nephrotic?
nephritic
What age group is targeted for acute proliferative glomerulonephritis?
pediatrics (but can occur at any age)
What is clinically seen in acute proliferative glomerulonephritis?
- usually comes about 1-4 weeks after acute infection (usu pharnygeal or skin)
- non-infectious; immunologically mediated (at this point, infection as resolved so we won’t see organism in urine)
- sub-epithelial immune complexes (anti-strep Abs -> Ag-Ab complex forms -> deposit in glomeruli -> triggers 2O immune-mediated response)
- low complement
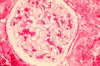
What is seen in H&E stains of acute proliferative glomerulonephritis?
- neutrophils plugging up glomerular lumens
- cells have multi-lobed nuclei
- cannot distinguish epithelial from mesangial from endothelial etc.
- marked hypercellularity (many black dots)
- structural loss

What is expected in FM of acute proliferative glomerulonephritis?
huge chunks of varying sizes

What is expected in EM of acute proliferative glomerulonephritis?
large, irregular clumps on sub-epithelial side of BMl - don’t distort BM!